Causes | Symptoms | Diagnosis | Treatment | Complications | Prevention | FAQs
Toxoplasmosis is a common and potentially serious parasitic infection caused by the protozoan parasite Toxoplasma gondii. It can affect both humans and animals, and its prevalence worldwide makes it a significant health concern.
What is toxoplasmosis?
Toxoplasmosis is a zoonotic parasitic disease caused by the protozoan parasite Toxoplasma gondii, which is transmitted from infected cats to humans. While many individuals may contract this parasite at some point in their lives, the majority experience mild or no symptoms. However, for certain vulnerable populations, such as pregnant women and individuals with compromised immune systems, toxoplasmosis can lead to severe complications.
What are the causes of toxoplasmosis?
Toxoplasmosis is primarily caused by the microscopic parasite Toxoplasma gondii. This parasite can be found in various environments, but its primary hosts are cats and other members of the Felidae family. Infection occurs when humans or animals come into contact with the parasite through:
- Ingestion of Contaminated Food or Water: Consuming food or water contaminated with Toxoplasma gondii is one of the most common ways people become infected. This can occur when fruits, vegetables, or meat are contaminated with oocysts (the parasite’s infectious form). Improperly cooked or undercooked meat, especially pork, lamb, and venison, can carry the parasite. Contaminated water sources can also be a source of infection.
- Handling Cat Litter: Toxoplasma gondii can be shed in the feces of infected cats. Cleaning a cat’s litter box without proper hand hygiene can lead to infection if the parasite is ingested accidentally. Pregnant women and individuals with weakened immune systems should avoid cleaning cat litter to reduce the risk of infection.

- Contact with Soil or Sand: Soil and sand can become contaminated with Toxoplasma gondii oocysts from cat feces. Gardening or playing in soil or sand without proper handwashing afterward can increase the risk of infection.
- Consuming Contaminated Raw Milk: Drinking raw, unpasteurized milk from infected animals can transmit the parasite. Proper pasteurization kills the parasite and makes milk safe for consumption.
- Organ Transplant or Blood Transfusion: In rare cases, Toxoplasma gondii can be transmitted through organ transplantation or blood transfusion if the donated organ or blood is infected with the parasite. This is more likely to occur when donors are not screened for toxoplasmosis.
- Vertical Transmission: Pregnant women who become infected with Toxoplasma gondii can pass the infection to their developing fetus. This can lead to congenital toxoplasmosis, which may cause birth defects or developmental problems in the baby. The risk of transmission depends on several factors, including the gestational age at which the mother acquires the infection. The earlier in pregnancy the infection occurs, the higher the risk of vertical transmission.
- Laboratory Accidents: Although uncommon, laboratory workers who handle the parasite for research purposes can accidentally become infected if they do not follow proper safety protocols.
What are the symptoms of toxoplasmosis?
Toxoplasmosis can manifest with a wide range of symptoms, and in some cases, it may remain asymptomatic. The severity of the disease largely depends on the individual’s immune status and the stage of infection.
Asymptomatic infection:
Many people who become infected with Toxoplasma gondii do not experience any symptoms at all. Their immune systems effectively control the infection, and the parasite remains dormant in the body. These individuals are considered asymptomatic carriers.
Flu-like symptoms:
In some cases, especially in healthy individuals, the initial infection may lead to mild flu-like symptoms, such as fatigue, headache, muscle aches, and fever. These symptoms can be mistaken for other common illnesses, making toxoplasmosis difficult to diagnose based solely on clinical presentation. They include;

- Fever: Fever is a common symptom of toxoplasmosis. During the acute phase of the infection, individuals may experience an increase in body temperature. This fever is usually low-grade, with temperatures ranging from 100°F (37.8°C) to 102°F (38.9°C). It can last for several days to a few weeks.
- Fatigue: Profound tiredness and weakness, often referred to as fatigue, are frequently reported by individuals with toxoplasmosis. This symptom can be debilitating and may persist even after the fever subsides.
- Headache: Headaches are another common flu-like symptom associated with toxoplasmosis. These headaches can range from mild to severe and may be accompanied by sensitivity to light (photophobia) or sound.
- Muscle Aches: Muscular discomfort and aching, often similar to what one experiences during the flu, can be present. This symptom can contribute to overall discomfort and fatigue.
- Sore Throat: A sore throat, along with other flu-like symptoms, may occur in some cases. It can be a mild irritation or more severe, depending on the individual’s immune response.
Swollen lymph nodes:
Swollen lymph nodes, a condition known as lymphadenopathy, can be one of the notable symptoms. Enlarged lymph nodes associated with toxoplasmosis are typically painless. Unlike swollen lymph nodes caused by bacterial infections, which can be tender and painful, those affected by toxoplasmosis usually do not cause discomfort. They often persist for several weeks, as the immune system continues to combat the infection. However, they should gradually decrease in size as the infection is controlled or treated.
Ocular symptoms:
Toxoplasmosis can affect the eyes, leading to symptoms like blurred vision, eye pain, redness, and sensitivity to light (photophobia). This condition is called ocular toxoplasmosis and can cause permanent damage to the retina if left untreated.
Severe symptoms:
- Immunocompromised individuals, such as those with HIV/AIDS, cancer patients undergoing chemotherapy, and organ transplant recipients on immunosuppressive medications, are at higher risk of developing severe toxoplasmosis.
- In these cases, the parasite can reactivate and cause more severe symptoms. These may include confusion, seizures, poor coordination, and even coma, as the parasite can invade the central nervous system.
Congenital toxoplasmosis:
- When pregnant women become infected with Toxoplasma gondii, the parasite can be transmitted to the developing fetus. This can lead to congenital toxoplasmosis, which may cause a range of symptoms in newborns, including jaundice, seizures, rash, and enlarged liver and spleen.
- These infants may also develop eye problems and developmental delays over time.
How is toxoplasmosis diagnosed?
Diagnosing toxoplasmosis can be a complex process due to the wide range of symptoms or the possibility of asymptomatic infection. The diagnostic approach varies depending on the individual’s clinical presentation and risk factors.
Clinical evaluation:
The first step in diagnosing toxoplasmosis is often a thorough clinical evaluation by a healthcare provider. They will inquire about the patient’s medical history, symptoms, and potential risk factors for infection. It’s essential to assess the patient’s risk factors, such as exposure to cats, consumption of undercooked meat, or travel to regions with a higher prevalence of the parasite. This information can help guide the diagnostic process.
Serological testing:
Serological tests are the most commonly used diagnostic tools for toxoplasmosis. These tests detect antibodies produced by the immune system in response to the Toxoplasma gondii parasite. There are two primary types of antibodies that can be detected:
- IgM Antibodies: These antibodies appear early in the infection and can be detected within the first few weeks. A positive IgM test suggests recent or acute infection.
- IgG Antibodies: IgG antibodies develop later and can persist for years, indicating a past or chronic infection.
The most common serological tests include enzyme-linked immunosorbent assays (ELISA) and indirect fluorescent antibody tests (IFA). Positive serological tests, particularly IgM, are strong indicators of toxoplasmosis.
Polymerase chain reaction (PCR):
- PCR is a molecular technique used to detect the presence of Toxoplasma gondii DNA in various clinical specimens, such as blood, cerebrospinal fluid, or tissue samples.
- PCR is particularly useful for diagnosing congenital toxoplasmosis or when there is central nervous system involvement.
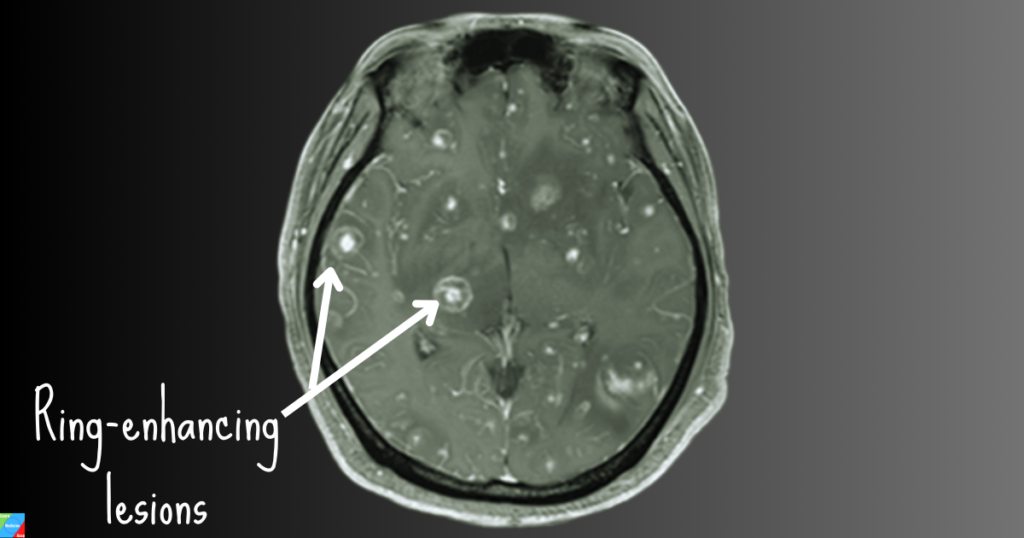
Imaging studies:
In cases of suspected ocular toxoplasmosis or neurological involvement, imaging studies such as computed tomography (CT) scans or magnetic resonance imaging (MRI) may be performed to visualize any lesions or abnormalities in the affected organs, such as the eyes or brain.
Biopsy:
In some cases, a tissue biopsy may be necessary to confirm the presence of Toxoplasma gondii in specific organs. Biopsies are typically performed when there is a suspicion of severe disease or when other diagnostic methods are inconclusive.
Amniotic fluid testing:
In pregnant women with suspected congenital toxoplasmosis, amniotic fluid testing may be conducted to assess whether the fetus has been infected. This involves obtaining a sample of amniotic fluid and performing PCR or serological tests on it.
Immunohistochemistry:
Immunohistochemistry is a specialized technique used to detect Toxoplasma gondii antigens in tissue samples. It is often employed in cases where a tissue biopsy is performed.
Differential diagnosis:
Infections:
- Cytomegalovirus (CMV) Infection
- HIV/AIDS-related opportunistic infections
Central nervous system (CNS) infections:
- Cryptococcal Meningitis
- Bacterial or Fungal Brain Abscesses
Autoimmune conditions:
- Multiple Sclerosis (MS)
- Systemic Lupus Erythematosus (SLE)
Neoplastic conditions:
- Primary or Metastatic Brain Tumors
- Lymphoma
Inflammatory conditions:
Temporal Arteritis (Giant Cell Arteritis)
How is toxoplasmosis treated?
The treatment of toxoplasmosis depends on the severity of the infection, the individual’s immune status, and the specific clinical manifestations.
No treatment (Observation):
- In many cases, especially among immunocompetent individuals (those with a healthy immune system), toxoplasmosis may resolve on its own without specific treatment.
- For mild or asymptomatic cases, healthcare providers may choose a “watch and wait” approach to monitor the progression of the infection.
Antiparasitic medications:
When treatment is necessary, antiparasitic medications are the primary approach to managing toxoplasmosis. These medications work to kill or inhibit the replication of Toxoplasma gondii. Commonly used drugs include:
- Pyrimethamine: Pyrimethamine is the most frequently prescribed medication for toxoplasmosis. It inhibits the parasite’s ability to replicate by blocking the synthesis of folate, an essential nutrient for the parasite.
- Sulfadiazine: Sulfadiazine is often used in combination with pyrimethamine. It enhances the effectiveness of pyrimethamine and helps prevent resistance.
- Leucovorin (Folinic Acid): Leucovorin is often administered alongside pyrimethamine to counteract potential side effects and complications, such as bone marrow suppression and megaloblastic anemia.
The duration of treatment with these medications can vary, but it is typically continued for several weeks to a few months, depending on the severity of the infection and the patient’s response.
Treatment for ocular toxoplasmosis:
Ocular toxoplasmosis, which affects the eyes, is usually treated with antiparasitic medications as mentioned above. In some cases, corticosteroids may also be prescribed to reduce inflammation in the eyes.
Treatment for severe or central nervous system involvement:
- Severe toxoplasmosis cases, especially those involving the central nervous system (CNS), may require more intensive treatment.
- In CNS involvement, medications like pyrimethamine and sulfadiazine are often used in combination with leucovorin. Additionally, corticosteroids may be administered to reduce inflammation and manage symptoms.
Management of congenital toxoplasmosis:
- Congenital toxoplasmosis, which affects infants born to mothers infected during pregnancy, may require a combination of medications, including pyrimethamine and sulfadiazine. Treatment is typically initiated promptly to minimize the risk of severe complications.
- Infants with congenital toxoplasmosis may also undergo regular monitoring and follow-up evaluations.
What are the complications of toxoplasmosis?
While toxoplasmosis is usually mild, it can lead to severe complications in certain cases, particularly if left untreated. The following are potential complications associated with toxoplasmosis:
Ocular complications:
- Chorioretinitis: Ocular toxoplasmosis is a common complication where the parasite affects the eyes, often causing chorioretinitis. This condition involves inflammation and damage to the retina, which can lead to vision impairment or loss if left untreated.
- Glaucoma: In some cases, ocular toxoplasmosis can lead to increased intraocular pressure, resulting in glaucoma, a condition that can further damage the optic nerve and impair vision.
- Scarring: Repeated or severe episodes of ocular toxoplasmosis can result in scarring in the eye, which may lead to permanent visual impairment.
Neurological complications:
- Encephalitis: Toxoplasmosis can affect the central nervous system, leading to encephalitis (inflammation of the brain). This condition can cause symptoms such as confusion, seizures, headaches, and altered mental status. Encephalitis can be life-threatening, especially in individuals with compromised immune systems.
- Meningitis: Inflammation of the meninges, the protective membranes surrounding the brain and spinal cord, can occur as a result of toxoplasmosis, leading to meningitis. Symptoms may include severe headaches, neck stiffness, and fever.
Cardiac complications:
Myocarditis: In rare cases, toxoplasmosis can cause inflammation of the heart muscle (myocarditis), leading to symptoms such as chest pain, palpitations, and shortness of breath. Severe myocarditis can compromise cardiac function.
Pulmonary complications:
Pulmonary infiltrates: Toxoplasmosis can affect the lungs, causing pulmonary infiltrates and respiratory symptoms. These symptoms may include cough, chest pain, and difficulty breathing.
Complications in pregnant women and newborns:
- Congenital toxoplasmosis: When a pregnant woman becomes infected with Toxoplasma gondii, the parasite can cross the placenta and infect the developing fetus. Congenital toxoplasmosis can result in a range of complications in newborns, including intellectual disabilities, visual impairment, hearing loss, seizures, and developmental delays.
- Miscarriage or stillbirth: Severe cases of congenital toxoplasmosis can lead to miscarriage or stillbirth.
Reactivation in immunocompromised individuals:
- HIV/AIDS patients: Individuals with HIV/AIDS are at particular risk of developing severe toxoplasmosis. The parasite can reactivate in these individuals due to their weakened immune system, leading to potentially life-threatening complications, such as encephalitis.
- Organ transplant recipients: Patients who have received organ transplants and are on immunosuppressive medications are also at risk of toxoplasmosis reactivation.
Systemic symptoms in immunocompromised individuals:
Immunocompromised individuals may experience a wide range of systemic symptoms, including fever, fatigue, weight loss, and generalized malaise, as the parasite can disseminate throughout the body.
Recurrence and chronic infection:
Toxoplasmosis can sometimes become a chronic infection, with recurring episodes of symptoms, especially in individuals with weakened immune systems. These recurrences can lead to ongoing health challenges.
How is toxoplasmosis prevented?
Toxoplasmosis prevention primarily involves adopting good hygiene practices and making informed choices to minimize exposure to the parasite.
Food safety:
- Cook meat thoroughly: Toxoplasma gondii can be present in undercooked or raw meat, particularly lamb, pork, and venison. To kill the parasite, it’s crucial to cook meat to a safe internal temperature.
- Freeze meat: Freezing meat at temperatures of -4°F (-20°C) or lower for at least 48 hours can also kill the parasite.
Safe food handling:
- Wash hands: Always wash your hands thoroughly with soap and water after handling raw meat, unwashed fruits and vegetables, or soil. Hand hygiene is crucial to prevent the transfer of the parasite to your mouth.
- Wash produce: Rinse fruits and vegetables under running water to remove soil and potential contamination. Scrub them, when necessary, but avoid using detergents or bleach.
- Use separate cutting boards: Use separate cutting boards and utensils for raw meat and other foods to prevent cross-contamination.
Cat litter and gardening:
- Avoid changing cat litter: Pregnant women should avoid changing cat litter whenever possible. If you must change it, wear disposable gloves and wash your hands thoroughly afterward.
- Gardening safety: Wear gloves while gardening to minimize contact with soil potentially contaminated with cat feces. Wash your hands afterward.
- Keep cats indoors: Reducing your cat’s exposure to outdoor environments can decrease the risk of infection.
Safe drinking water:
Ensure that your drinking water comes from a safe source and is properly treated. Toxoplasma cysts can contaminate water supplies, especially from surface water sources.
Avoid raw or unpasteurized products:
Avoid consuming raw or unpasteurized milk, cheeses, and dairy products, as these can harbor the parasite.
Regular pet care:
Maintain regular veterinary care for your pets, including routine deworming, to reduce the chances of them shedding the parasite.
Pregnant women:
- Avoid handling cat litter.
- Wear gloves when gardening or handling soil.
- Cook meat thoroughly and practice food safety.
- Wash hands frequently and avoid touching the face, especially after handling potentially contaminated items.
Frequently Asked Questions
Q: How common is toxoplasmosis?
A: Toxoplasmosis is relatively common, with about one-third of the global population estimated to have been exposed to the parasite. However, not everyone exposed to Toxoplasma gondii will develop symptoms.
Q: How is toxoplasmosis transmitted?
A: Toxoplasmosis can be transmitted through various routes, including consuming undercooked or raw meat containing the parasite, ingesting contaminated food or water, handling infected cat litter or soil, from mother to baby during pregnancy, and rarely, through organ transplantation or blood transfusion.
Q: What are the symptoms of toxoplasmosis in humans?
A: Symptoms of Toxoplasmosis can vary widely. Common symptoms include fever, muscle aches, and fatigue. Severe cases can lead to eye problems and brain inflammation, especially in individuals with weakened immune systems.
Q: Can toxoplasmosis be cured?
A: Yes, Toxoplasmosis can be treated with antibiotics, usually a combination of pyrimethamine and sulfadiazine. Timely treatment is particularly crucial for pregnant women and those with weakened immune systems.
Q: Can I get toxoplasmosis from my pet cat?
A: While it’s possible, the risk is generally low. Practicing good hygiene, like cleaning the cat’s litter box daily and washing hands afterward, can reduce the risk. Pregnant women and those with weakened immune systems should take extra precautions.
Q: Is toxoplasmosis more dangerous for pregnant women?
A: Yes, toxoplasmosis can pose a greater risk to pregnant women, as it can lead to congenital toxoplasmosis, which may harm the fetus.
Q: Are there any long-term complications of toxoplasmosis?
A: In healthy individuals, Toxoplasmosis typically resolves without long-term complications. However, in severe cases or in those with compromised immune systems, it can lead to serious health issues, including eye problems and brain damage.
Q: Is there a vaccine for toxoplasmosis?
A: Currently there is no commercially available vaccine for Toxoplasmosis. Research was ongoing, but no vaccines had been approved for general use.
Take-home message
Toxoplasmosis is a widespread parasitic infection that can affect anyone, but with awareness and preventive measures, the risk of infection can be significantly reduced. Understanding its causes, symptoms, prevention, and treatment is essential for both healthcare professionals and the general public. By following proper hygiene practices and seeking medical care when necessary, we can mitigate the impact of this potentially serious infection and promote overall health and well-being.
References
- Dubey, J. P. (2010). Toxoplasmosis of Animals and Humans (Second Edition). CRC Press.
- Robert-Gangneux, F., & Dardé, M. L. (2012). Epidemiology of and Diagnostic Strategies for Toxoplasmosis. Clinical Microbiology Reviews, 25(2), 264-296.
- Centers for Disease Control and Prevention (CDC). “Toxoplasmosis – General Information.” Link