Types | Mode of Transmission | Symptoms | Diagnosis | Treatment | Complications | Prevention | FAQs
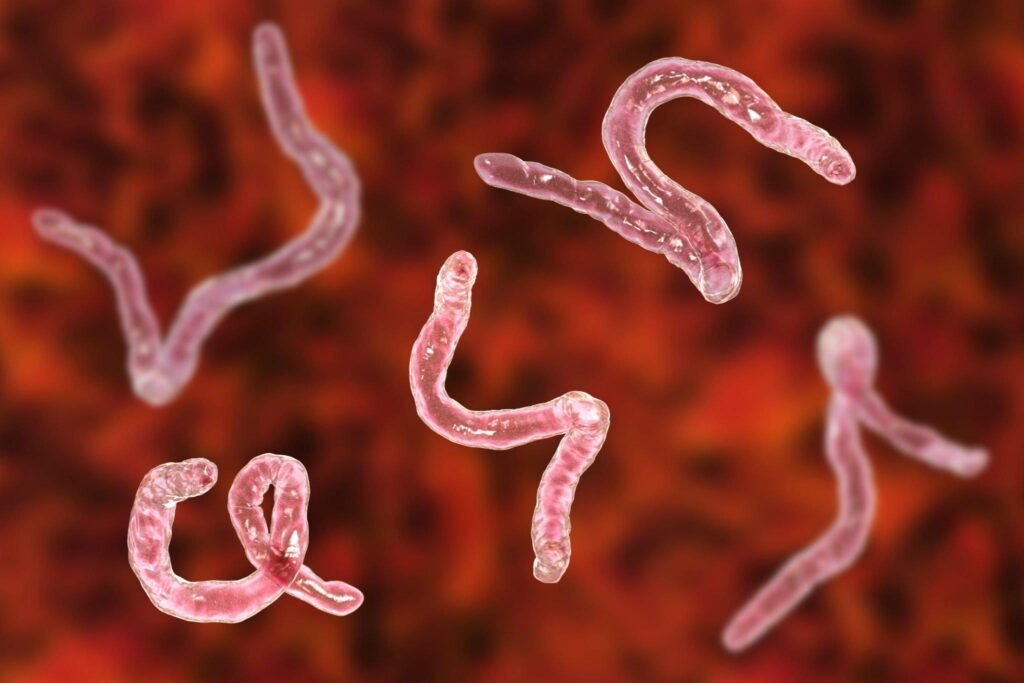
Hookworms are intestinal parasites that infect humans and animals. These parasites are transmitted through contaminated soil and can lead to various health problems if left untreated.
What is hookworm infection?
Hookworm Infection is a parasitic disease caused by hookworms, primarily the Ancylostoma duodenale and Necator americanus species. These minuscule worms, measuring just a few centimeters in length, may seem harmless, but they can wreak havoc in the human body.
What are the types of hookworms?
Hookworms are a group of parasitic nematode worms that belong to the family Ancylostomatidae. These worms are commonly found in the intestines of mammals, including humans, and they can cause a variety of health problems when they infect their hosts. There are several species of hookworms that affect humans, with two of the most significant ones being Ancylostoma duodenale and Necator americanus.
Ancylostoma duodenale:
- Common Name: This species is often referred to as the “Old World hookworm” or simply the “hookworm.”
- Distribution: Ancylostoma duodenale is found primarily in regions of the Old World, including parts of Africa, Asia, and Southern Europe.
- Morphology: Adult Ancylostoma duodenale worms are relatively small, measuring about 1 cm in length. They have a characteristic hook-like mouthpart, which they use to attach to the lining of the small intestine.
- Lifecycle: The life cycle of Ancylostoma duodenale involves the passage of eggs in the host’s feces. These eggs hatch into larvae in the soil, and infection occurs when these larvae penetrate the skin of a human host, typically through bare feet. The larvae then migrate through the bloodstream to the lungs and are subsequently coughed up and swallowed, eventually reaching the small intestine, where they mature into adults.
- Health Implications: Ancylostoma duodenale infection can lead to a condition known as hookworm disease, which includes symptoms such as abdominal pain, diarrhea, anemia, and malnutrition. Severe infections can be particularly harmful to children and pregnant women.
Necator americanus:
- Common Name: Necator americanus is commonly referred to as the “New World hookworm.”
- Distribution: This species is predominantly found in the Americas, including regions of the United States, South America, and the Caribbean.
- Morphology: Similar to Ancylostoma duodenale, adult Necator americanus worms are relatively small, measuring around 1 cm in length. They also possess a hook-like mouthpart for attachment to the intestinal lining.
- Lifecycle: The life cycle of Necator americanus is similar to that of Ancylostoma duodenale. The larvae enter the host through the skin, migrate to the lungs, and then travel to the small intestine, where they mature into adults.
- Health Implications: Infections with Necator americanus can lead to a condition called “hookworm anemia” due to the worms’ blood-feeding behavior. Symptoms may include fatigue, weakness, and pallor. Chronic infections can impair physical and cognitive development in children.
How are hookworm infections spread?
Hookworm infections are typically spread through several key pathways:
Contaminated Soil: The primary mode of transmission for hookworm infections is through contact with soil contaminated with hookworm larvae. The lifecycle of hookworms involves the shedding of eggs in the feces of infected individuals. These eggs hatch into larvae in the soil, and when conditions are favorable, they become infectious and can penetrate the skin of individuals who come into contact with contaminated soil.
Barefoot Walking: Walking barefoot on soil or surfaces contaminated with hookworm larvae is a common cause of infection. The larvae can penetrate the skin, usually through the feet, and enter the bloodstream. From there, they migrate to the lungs and are eventually swallowed, reaching the small intestine, where they mature into adult worms.
Poor Sanitation: In regions with inadequate sanitation facilities, human feces containing hookworm eggs can contaminate the environment, including soil in areas where people defecate openly or where sewage is not properly managed. This increases the likelihood of hookworm larvae being present in the soil, posing a constant risk of infection to individuals in these areas.
Occupational Exposure: Certain occupations, such as agriculture, mining, and construction, may put individuals at a higher risk of hookworm infection due to prolonged exposure to contaminated soil. Workers in these industries may inadvertently come into contact with larvae while working without adequate protective measures.
Geographical Location: The prevalence of hookworm infections is often higher in tropical and subtropical regions with warm and humid climates. These conditions favor the survival and maturation of hookworm larvae in the soil, increasing the risk of infection for residents in these areas.
Personal Hygiene: Poor personal hygiene practices, such as not washing hands properly after using the restroom or before eating, can lead to the ingestion of hookworm larvae present on contaminated hands or surfaces. This ingestion route can also result in infection.
Contaminated Water: Although less common, hookworm larvae can survive in water sources contaminated with fecal matter. Ingesting or coming into contact with such contaminated water can lead to infection.
Vertical Transmission: Pregnant women with hookworm infections can transmit the parasites to their unborn children. This can occur when the larvae in the mother’s body migrate through the placenta and into the fetus. It can also happen through breastfeeding if the mother is infected.
What are the symptoms of hookworm infections?
Hookworm infections can lead to a range of symptoms and health problems. These symptoms typically result from the worms’ activities in the small intestine, where they attach themselves to the intestinal lining and feed on blood.
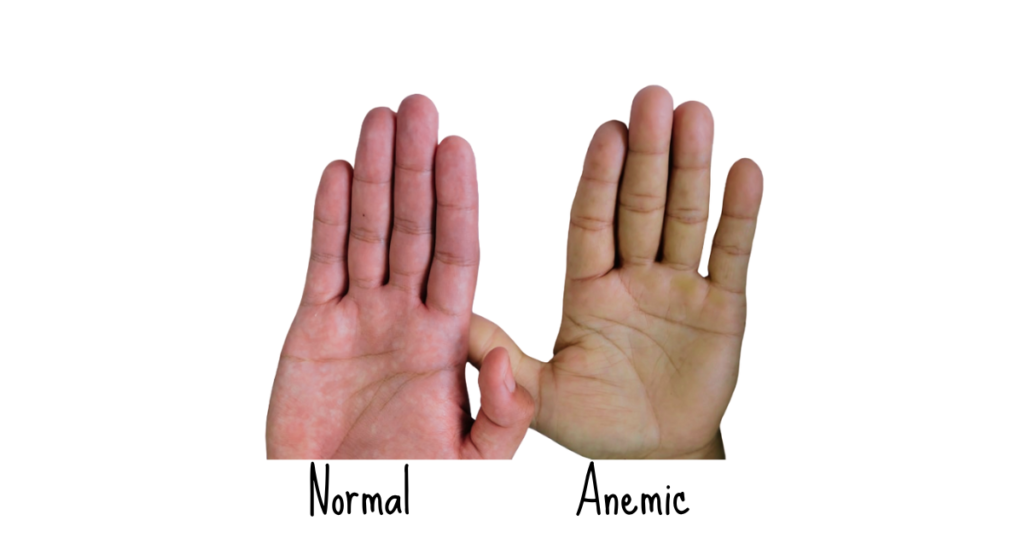
Anemia: One of the most common and significant symptoms of hookworm infection is anemia. The hookworms feed on the host’s blood by attaching themselves to the intestinal mucosa and releasing anticoagulants to prevent the blood from clotting. This chronic blood loss leads to a decrease in the number of red blood cells and a reduction in hemoglobin levels. Anemic individuals may experience fatigue, weakness, pale skin, and shortness of breath.
Gastrointestinal Symptoms: Hookworm infections can cause various gastrointestinal problems, including:
- Abdominal Pain: Individuals with hookworm infections often experience abdominal discomfort, cramps, and pain, which can range from mild to severe.
- Diarrhea: Chronic diarrhea is a common symptom, accompanied by loose stools and, in some cases, blood in the stool.
- Nausea and Vomiting: Some individuals may experience nausea and occasional vomiting.
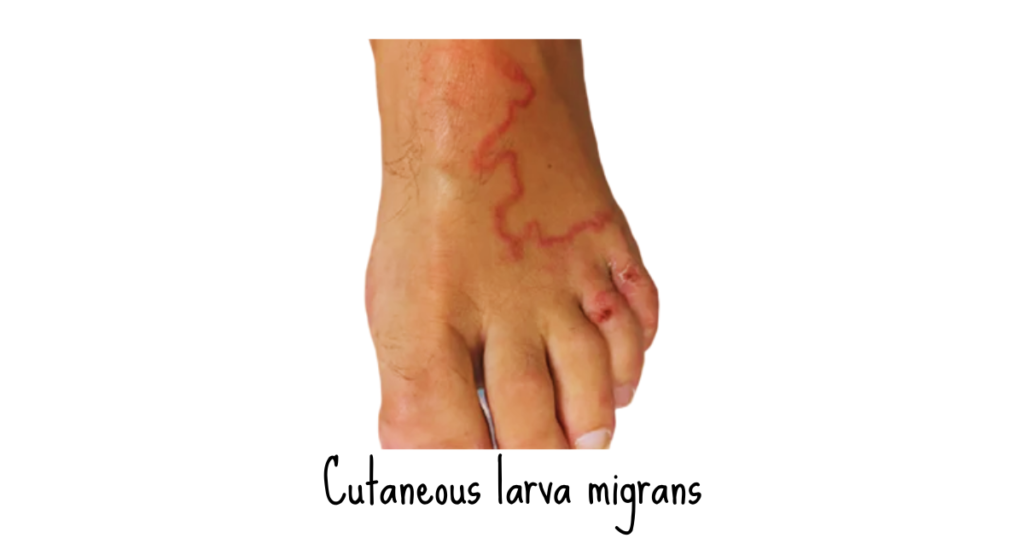
Skin Rash and Itching: In some cases, hookworm larvae can penetrate the skin, causing an itchy, red rash known as “creeping eruption” or “cutaneous larva migrans.” This condition occurs when the larvae migrate under the skin but fail to reach the lungs and the small intestine.
Loss of Appetite: Hookworm infections can lead to a decreased appetite, which, if prolonged, can result in weight loss and malnutrition.
Iron Deficiency: Anemia resulting from hookworm infection can lead to iron deficiency, which can manifest as weakness, dizziness, and brittle nails.
Cognitive and Developmental Effects: In children, particularly those with chronic and severe infections, hookworms can cause cognitive and developmental impairments. Anemia and malnutrition can hinder a child’s physical and mental growth, potentially leading to learning difficulties and developmental delays.
Peripheral Edema: In some cases, individuals with severe hookworm infections may develop peripheral edema, a condition characterized by swelling of the legs and feet due to fluid retention.
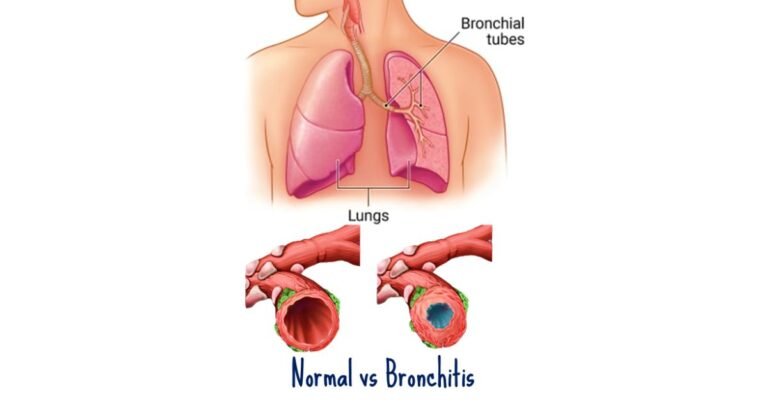
Respiratory Symptoms: During their migration through the body, hookworm larvae can pass through the lungs, causing symptoms such as coughing, wheezing, and mild respiratory discomfort.
How are hookworm infections diagnosed?
Diagnosing hookworm infections involves a combination of clinical evaluation, laboratory tests, and sometimes imaging studies. Accurate diagnosis is essential for proper management and treatment of the infection.
Clinical Evaluation:
- Medical History: The healthcare provider will start by taking a detailed medical history, including questions about symptoms, recent travel to endemic areas, and any previous exposure to contaminated soil.
- Physical Examination: A physical examination may reveal signs associated with hookworm infection, such as pallor (pale skin), fatigue, abdominal pain, and, in severe cases, edema (swelling) of the legs and feet.
Stool Examination:
Direct Fecal Smear: The most common diagnostic method for hookworm infections is a microscopic examination of stool samples. A small amount of fresh feces is examined under a microscope to detect the presence of hookworm eggs. This method may require multiple stool samples collected over several days to increase the chances of detection, as egg shedding can be intermittent.
Blood Tests:
- Complete Blood Count (CBC): A CBC can help diagnose hookworm infections by revealing characteristic findings of anemia, such as a decreased red blood cell count and low hemoglobin levels. Elevated eosinophil levels may also indicate parasitic infections.
- Iron Studies: Measuring serum ferritin levels can help confirm iron deficiency anemia, which is commonly associated with hookworm infections.
Serological Tests:
In some cases, serological tests may be used to detect specific antibodies produced by the host in response to hookworm infection. These tests, such as ELISA (enzyme-linked immunosorbent assay), can be particularly helpful in cases where stool examinations are inconclusive or when evaluating travelers who may have been exposed to hookworms.
Imaging Studies:
In cases where hookworm larvae migrate through the lungs and cause respiratory symptoms, chest X-rays or CT scans may be performed to visualize any abnormalities in the lungs. This can help confirm the presence of larvae.
Endoscopy:
In rare cases, endoscopy may be used to directly visualize the small intestine for the presence of adult hookworms or related lesions. This method is invasive and typically reserved for cases with severe symptoms or complications.
What is the treatment of hookworm infections?
The treatment of hookworm infections involves the use of antiparasitic medications to eliminate the adult worms and larvae from the intestines. Additionally, supportive measures may be necessary to address complications like anemia.
Antiparasitic Medications:
- Albendazole: Albendazole is a commonly used medication for treating hookworm infections. It works by interfering with the parasites’ ability to absorb glucose, leading to their death. A typical course of treatment with albendazole is a single oral dose of 400 milligrams.
- Mebendazole: Mebendazole is another effective antiparasitic medication used to treat hookworm infections. It works by disrupting the parasites’ ability to absorb nutrients. The standard regimen for mebendazole is a single oral dose of 500 milligrams.
- Pyrantel Pamoate: Pyrantel pamoate is an alternative medication that can be used to treat hookworm infections. It paralyzes the worms, allowing them to be expelled from the intestines through normal bowel movements. The dosing may vary depending on the specific product used, and it is typically administered as a single dose.
Iron Supplements:
- In cases where hookworm infection has led to anemia due to chronic blood loss, iron supplements may be prescribed to address the deficiency. Iron supplements can help restore hemoglobin levels and alleviate symptoms of anemia, such as fatigue and weakness.
Hydration and Nutritional Support:
- In severe cases of hookworm infection, especially when there is malnutrition or dehydration, intravenous (IV) fluids and nutritional support may be necessary. Hospitalization may be required for individuals with complications.
Monitoring and Follow-Up:
- Individuals who have been treated for hookworm infections should be monitored for the resolution of symptoms and improvement in hemoglobin levels. Follow-up stool examinations may also be performed to confirm the elimination of the parasites.
- It’s essential to educate patients about preventive measures to avoid reinfection, such as wearing shoes, practicing good hygiene, and improving sanitation in endemic areas.
Mass Drug Administration (MDA):
- In areas with a high prevalence of hookworm infections, public health interventions may involve mass drug administration campaigns. These campaigns aim to treat entire communities or populations at risk with antiparasitic medications to reduce the burden of infection and prevent transmission.
What are the complications of hookworm infections?
Hookworm infections can lead to various complications, especially when left untreated or when the infections become chronic. These complications can have a significant impact on an individual’s health and well-being.
Anemia: Anemia is one of the most common and significant complications of hookworm infections. The parasites attach to the lining of the small intestine and feed on blood. Over time, this chronic blood loss can lead to a decrease in the number of red blood cells and a reduction in hemoglobin levels. Anemic individuals may experience fatigue, weakness, pallor (pale skin), and shortness of breath.
Malnutrition: Hookworms contribute to malnutrition by impairing the host’s ability to absorb essential nutrients from the intestines. Chronic infections can lead to deficiencies in vital nutrients such as iron, vitamin B12, and protein. This can result in weight loss, stunted growth (especially in children), and weakened immune function.
Cognitive and Developmental Impairments: In children, particularly those with chronic and severe hookworm infections, malnutrition and anemia can hinder physical and cognitive development. This can lead to learning difficulties, developmental delays, and long-term consequences for educational and economic opportunities.
Edema: In severe cases, individuals with hookworm infections may develop peripheral edema, which is characterized by the swelling of the legs and feet. Edema results from the body’s attempt to retain fluids in response to anemia and hypoalbuminemia (low levels of albumin in the blood).
Respiratory Symptoms: During their migration through the body, hookworm larvae can pass through the lungs, causing respiratory symptoms such as coughing, wheezing, and mild respiratory discomfort. This is more common in heavily infected individuals.
Secondary Infections: Scratching and skin irritation caused by larval penetration through the skin can lead to bacterial skin infections, which can worsen the overall health of the infected person.
Complications in Pregnant Women: Pregnant women with hookworm infections are at increased risk of complications such as low birth weight and premature birth. The anemia associated with hookworm infections can further exacerbate these risks.
Increased Susceptibility to Other Infections: Hookworm infections can weaken the immune system, making individuals more susceptible to other infections and illnesses.
How can you prevent hookworm infections?
Preventing hookworm infections involves a combination of public health measures, personal hygiene practices, and community education efforts. Here are some strategies to protect yourself:
Improving Sanitation:
- Access to clean and safe sanitation facilities, such as toilets and latrines, is a crucial step in preventing hookworm infections. These facilities help contain human feces and prevent the contamination of soil with hookworm eggs.
- Promoting the use of toilets and discouraging open defecation can significantly reduce the risk of soil contamination with hookworm larvae.
Hygiene Education:
Community education programs should focus on raising awareness about the importance of good hygiene practices. This includes teaching individuals to:
- Wash their hands thoroughly with soap and clean water after using the toilet and before eating.
- Avoid walking barefoot on soil or surfaces that may be contaminated with hookworm larvae.
Wearing Shoes:
- Encouraging the use of shoes or sandals in areas with a high risk of soil contamination can greatly reduce the risk of hookworm infection. Providing affordable or donated footwear to vulnerable populations is a practical intervention.

Proper Disposal of Fecal Waste:
- Ensuring proper disposal of human and animal feces is essential to prevent soil contamination. Waste should be disposed of in designated sanitary systems, such as pit latrines or sewage systems.
Mass Drug Administration (MDA):
- In endemic areas with a high prevalence of hookworm infections, public health interventions may involve mass drug administration campaigns. These campaigns aim to treat entire communities or populations at risk with antiparasitic medications, reducing the overall burden of infection and preventing further transmission.
Soil Treatment:
- In some cases, soil treatment with chemicals or heat may be employed in endemic areas to kill hookworm larvae present in the soil. However, this is a less common and more resource-intensive approach.
Regular Deworming Programs:
- Implementing regular deworming programs in schools and communities can help reduce the prevalence of hookworm infections, particularly among children who are most vulnerable. Schools may provide anthelmintic medications to students at scheduled intervals.
Improving Access to Safe Drinking Water:
- Ensuring access to clean and safe drinking water sources can reduce the risk of infection, as hookworm larvae can survive in contaminated water. Communities should have access to treated and safe water supplies.
Community Engagement:
- Engaging local communities in the prevention efforts is crucial. Community members can play an active role in maintaining sanitation facilities, practicing good hygiene, and supporting mass drug administration programs.
Health Education and Awareness:
- Public health campaigns and educational materials should be developed and distributed to raise awareness about hookworm infections, their transmission, and prevention measures.
Frequently Asked Questions
Q: How do people get infected with hookworms?
A: People usually get infected with hookworms by walking barefoot on soil contaminated with hookworm larvae. The larvae can penetrate the skin and then migrate to the intestines.
Q: Can hookworms affect animals, or are they exclusive to humans?
A: Hookworms can infect both animals and humans. They are common parasites in pets like dogs and cats and can also affect livestock.
Q: Can animals transmit hookworm infections to humans?
A: Hookworm species that infect animals are generally not the same as those that infect humans. However, contact with contaminated animal feces can potentially lead to human infection in certain cases.
Q: How do hookworms cause anemia in infected individuals?
A: Hookworms attach themselves to the lining of the small intestine and feed on blood. Over time, this blood loss can lead to anemia, which is characterized by a decrease in red blood cell count and iron deficiency.
Q: Can hookworm infections be treated?
A: Yes, hookworm infections can be treated with antiparasitic medications such as albendazole or mebendazole. Iron supplements may also be given to address anemia.
Q: Can you get reinfected with hookworms after treatment?
A: Yes, reinfection is possible if an individual continues to be exposed to contaminated soil or feces. Proper sanitation and hygiene practices are crucial to preventing reinfection.
Q: Are there any natural remedies for Hookworm Infection?
A: While natural remedies may provide some relief from symptoms, they are not a substitute for medical treatment.
Q: Are there any long-term complications associated with untreated hookworm infections?
A: Yes, chronic hookworm infections can lead to severe anemia, malnutrition, stunted growth in children, and cognitive impairments. These complications can be especially detrimental in areas with high infection rates.
Q: What measures can travelers take to avoid hookworm infections in endemic areas?
A: Travelers should avoid walking barefoot, especially in rural or sandy areas, and should practice good hygiene, including thorough handwashing and avoiding consumption of untreated water and food.
Q: Can hookworm infections be prevented in pets?
A: Yes, regular deworming of pets is essential to prevent hookworm infections. Pet owners should also practice good hygiene when handling feces and maintain clean living conditions for their animals.
Q: Can Hookworm Infection be prevented through vaccination?
A: Currently, there is no vaccine available for Hookworm Infection. Prevention relies on hygiene and sanitation practices.
The Takeaway
Hookworm Infection is a parasitic condition that can be both concerning and uncomfortable. However, with the right knowledge and preventive measures, you can protect yourself and your loved ones. Remember to practice good hygiene, avoid contaminated water sources, and seek medical attention if you suspect an infection. By doing so, you can stay one step ahead of this pesky parasite.
References
- Jia, T. W., Melville, S., Utzinger, J., King, C. H., Zhou, X. N. (2012). Soil-transmitted helminth reinfection after drug treatment: a systematic review and meta-analysis. PLoS Neglected Tropical Diseases, 6(5), e1621. DOI: 10.1371/journal.pntd.0001621
- Hotez, P. J., & Pecoul, B. (2010). “Manifesto” for advancing the control and elimination of neglected tropical diseases. PLoS Neglected Tropical Diseases, 4(5), e718. DOI: 10.1371/journal.pntd.0000718
- World Health Organization (WHO). (2021). Soil-transmitted helminth infections. https://www.who.int/news-room/fact-sheets/detail/soil-transmitted-helminth-infections
- Centers for Disease Control and Prevention (CDC). (2021). Hookworm. https://www.cdc.gov/parasites/hookworm/index.html