What is malaria?
Types | Life Cycle | Symptoms | Diagnosis | Treatment | Complications | Prevention | Takeaway | FAQs
Malaria is a potentially life-threatening a vector-borne disease caused by parasites of the genus Plasmodium. This disease is primarily transmitted to humans through the bites of infected female Anopheles mosquitoes. This global health concern affects millions of people annually, particularly in tropical and subtropical regions.
What are the types of malaria Parasite?
Malaria is caused by parasites belonging to the genus Plasmodium, and several species within this genus are responsible for human infections. The most common types of malaria parasites that infect humans include:
- Plasmodium falciparum (P. falciparum): This species is the most severe and potentially fatal among the malaria parasites. P. falciparum is prevalent in tropical and subtropical regions and is responsible for the majority of malaria-related deaths. It is known for its ability to infect a high percentage of red blood cells, leading to rapid and severe complications if left untreated.
- Plasmodium vivax (P. vivax): P. vivax is another widespread malaria parasite, causing a significant number of infections globally. While it is generally less lethal than P. falciparum, P. vivax can remain dormant in the liver as hypnozoites, causing relapses of the infection months or even years after the initial mosquito bite. This characteristic adds complexity to the treatment and control of P. vivax malaria.
- Plasmodium ovale (P. ovale): P. ovale is less common than P. falciparum and P. vivax but can still cause malaria in humans. Similar to P. vivax, P. ovale can produce hypnozoites, leading to relapses. It is primarily found in West Africa.
- Plasmodium malariae (P. malariae): P. malariae is known for its chronic and long-lasting infections, often causing mild symptoms that persist for years. While it is generally less severe than P. falciparum, it can lead to complications such as nephrotic syndrome. P. malariae is distributed worldwide but is more prevalent in tropical regions.
- Plasmodium knowlesi (P. knowlesi): Originally considered a parasite of macaques, P. knowlesi has gained attention as a zoonotic malaria parasite capable of infecting humans. In some regions, particularly in Southeast Asia, P. knowlesi has been identified as a significant cause of human malaria, and its symptoms can range from mild to severe.
What is the Life Cycle of the malaria Parasite?
Malaria is primarily transmitted to humans through the bites of infected female Anopheles mosquitoes. The transmission cycle of malaria involves complex interactions between the human host and the mosquito vector. Here’s a detailed explanation of how malaria is transmitted:

- Infected mosquitoes: The cycle begins when female Anopheles mosquitoes, specifically those carrying the malaria parasites (Plasmodium species), bite an infected human. Only female mosquitoes bite as they require a blood meal to develop their eggs.
- Introduction of parasites: During the blood-feeding process, the infected mosquito injects sporozoites – the early stage of the malaria parasite – into the bloodstream of the human host. These sporozoites travel to the liver, where they invade liver cells and undergo a maturation process.
- Liver stage: Inside the liver cells, the sporozoites develop into schizonts, which then release merozoites. The merozoites can infect new liver cells, leading to the amplification of the parasite.
- Release into bloodstream: After the liver stage, the merozoites are released into the bloodstream. These newly formed parasites invade red blood cells, initiating the symptomatic phase of the infection.
- Asexual reproduction: Within red blood cells, the parasites undergo asexual reproduction, resulting in the release of more merozoites. This cycle of invasion, replication, and release causes the characteristic symptoms of malaria, including fever, chills, and anemia.
- Gametocytes formation: Some parasites differentiate into sexual forms called gametocytes, which circulate in the bloodstream. When another mosquito bites an infected human and ingests blood containing gametocytes, the cycle continues.
- Mosquitoes as vectors: Inside the mosquito’s stomach, gametocytes mature into gametes, forming male (microgametocytes) and female (macrogametocytes) gametes. Fertilization occurs, forming zygotes.
- Ookinete formation: The zygotes develop into ookinetes, which traverse the mosquito’s stomach wall and form oocysts on the outer surface. Within the oocysts, sporozoites are produced.
- Migration to salivary glands: The sporozoites migrate to the mosquito’s salivary glands, ready to be transmitted to another human during the mosquito’s next blood meal.
- Transmission to humans: When an infected mosquito bites another human, it injects sporozoites into the bloodstream, restarting the cycle.
What areas are prone to malaria?
Malaria is most prevalent in tropical and subtropical regions, where specific environmental conditions foster the breeding and survival of Anopheles mosquitoes—the primary vectors responsible for transmitting the Plasmodium parasites that cause malaria. The areas prone to malaria typically exhibit characteristics conducive to mosquito breeding and sustained transmission cycles.
- Climate: Malaria is more common in regions with warm temperatures and high humidity. The optimal conditions for malaria transmission occur in areas where temperatures remain consistently warm, typically between 20 to 30 degrees Celsius (68 to 86 degrees Fahrenheit).
- Rainfall: Adequate rainfall is essential for the creation and maintenance of breeding sites for Anopheles mosquitoes. Stagnant water, such as in puddles, ponds, and slow-flowing rivers, provides ideal breeding grounds for mosquito larvae. Heavy rainfall can create temporary breeding sites, contributing to increased mosquito populations.
- Altitude: Malaria transmission is generally limited to areas below a certain altitude. In higher-altitude regions, the cooler temperatures are less conducive to both mosquito survival and the development of the malaria parasite. As a result, malaria tends to be less prevalent in mountainous areas.
- Vegetation and land use: Areas with lush vegetation, forests, and significant water bodies often provide suitable habitats for mosquitoes. Deforestation and changes in land use can alter local ecosystems, creating environments that favor mosquito breeding.
- Population density: Malaria transmission is more likely in regions with high population density, as this increases the likelihood of contact between mosquitoes carrying the parasite and susceptible individuals. Urban areas with inadequate infrastructure for water management and sanitation may be particularly vulnerable.
- Vector species: The prevalence of specific Anopheles mosquito species capable of transmitting malaria varies by region. The presence of competent vectors is a critical factor in determining the risk of malaria transmission.
- Global distribution: Malaria is most endemic in sub-Saharan Africa, where the majority of global malaria cases and deaths occur. Other regions with a high burden of malaria include parts of Southeast Asia, the Indian subcontinent, Central and South America, and some areas in the Middle East.
What are the symptoms of malaria?
Malaria presents a spectrum of symptoms that can range from mild to severe, and the manifestations often depend on the species of the Plasmodium parasite causing the infection. The common symptoms of malaria typically appear 7 to 30 days after being bitten by an infected mosquito.
- Fever: Fever is one of the hallmark symptoms of malaria. It often begins with a sudden and pronounced rise in body temperature, accompanied by chills and shivering. The fever tends to occur in cycles, corresponding to the release of new generations of parasites into the bloodstream.
- Chills and sweats: Patients with malaria often experience episodes of intense cold followed by profuse sweating. These alternating chills and sweats are characteristic and contribute to the cyclical nature of the fever.
- Headache: Headaches are a common symptom of malaria, and they can range from mild to severe. The severity of the headache is often associated with the intensity of the fever.
- Muscle and joint pain: Malaria infections can cause generalized muscle and joint pain. This discomfort can contribute to a sense of overall malaise and fatigue.
- Nausea and vomiting: Many individuals with malaria experience nausea and may vomit. This can lead to a loss of appetite and contribute to dehydration, especially in severe cases.
- Fatigue and weakness: Malaria can induce a profound sense of fatigue and weakness, affecting the individual’s ability to carry out daily activities. This fatigue may persist even between episodes of fever.
- Anemia: In cases of prolonged or severe malaria, the destruction of red blood cells by the parasite can lead to anemia. Anemic individuals may experience symptoms such as pale skin, weakness, and shortness of breath.
- Jaundice: Severe malaria infections, particularly those caused by Plasmodium falciparum, can lead to jaundice. This condition is characterized by yellowing of the skin and eyes due to the breakdown of red blood cells and the release of bilirubin.
- Cognitive symptoms: In some cases, especially with severe forms of malaria, individuals may experience neurological symptoms such as confusion, seizures, and impaired consciousness. This is known as cerebral malaria and is a medical emergency requiring immediate attention.
It is important to note that the symptoms of malaria can mimic those of other infectious diseases, making accurate diagnosis crucial for effective treatment.
How is malaria diagnosed?
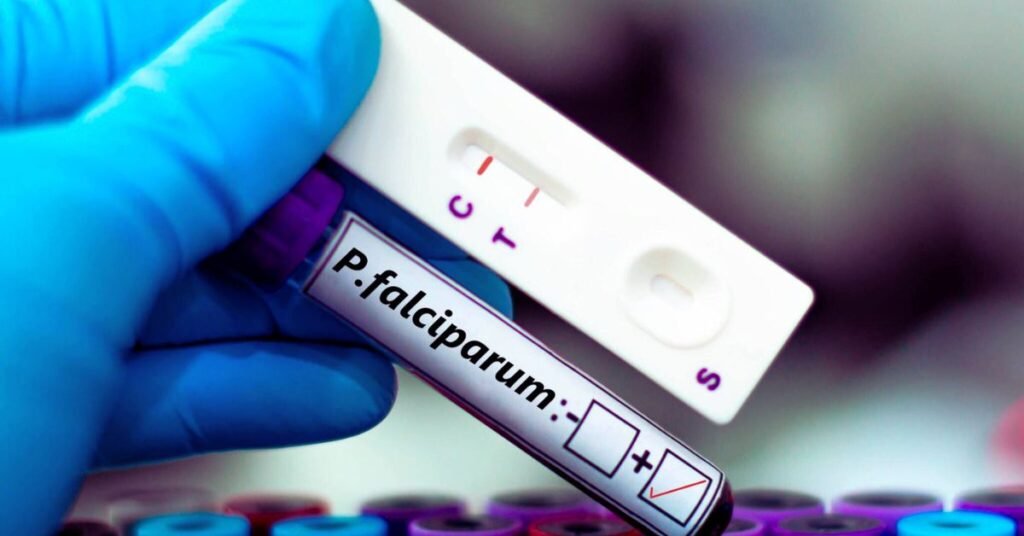
Several diagnostic methods are employed to identify the presence of Plasmodium parasites in the blood. The choice of diagnostic approach may depend on factors such as the availability of resources, the severity of the infection, and the specific context.
Microscopic examination of blood smears:
- Giemsa Staining: This traditional method involves preparing thin and thick blood smears on glass slides, which are then stained with Giemsa or a similar dye. Microscopic examination allows trained laboratory technicians to identify the presence of malaria parasites and determine the species.
- Thin Smear: A thin smear provides a detailed view of the parasites and is used for species identification.
- Thick Smear: A thick smear is more sensitive for detecting low-level parasitemia, making it useful in cases of low-level infections.
Rapid diagnostic tests (RDTs):
- RDTs are immunochromatographic tests that detect specific malaria antigens in a small blood sample. They are relatively easy to use and provide rapid results, making them particularly valuable in settings with limited laboratory infrastructure.
- RDTs are available for different Plasmodium species, with some tests specifically designed for the detection of P. falciparum or a combination of common species.
Nucleic acid-based tests:
- Polymerase Chain Reaction (PCR) and other nucleic acid amplification techniques are highly sensitive and specific methods for malaria diagnosis. These tests can detect and differentiate between various Plasmodium species.
- PCR is particularly useful in research settings and for confirming cases, especially when other diagnostic methods yield inconclusive results.
Antigen detection tests:
- Enzyme-Linked Immunosorbent Assay (ELISA) and other antigen detection tests can identify malaria antigens in blood samples. These tests are often used in research and surveillance settings.
Clinical assessment:
- In malaria-endemic areas, healthcare providers may rely on clinical symptoms and a history of potential exposure to malaria to make an initial diagnosis. However, clinical assessment alone is not sufficient for accurate diagnosis, as malaria symptoms can overlap with those of other diseases.
Accurate and prompt diagnosis is crucial for initiating appropriate antimalarial treatment and preventing severe complications.
How is malaria treated?
The treatment of malaria involves the administration of antimalarial drugs to eliminate the Plasmodium parasites causing the infection. The choice of antimalarial medication depends on several factors, including the species of the parasite, the severity of the infection, the patient’s age, and any potential drug resistance in the region.
Antimalarial drugs:
- Artemisinin-based combination therapies (ACTs): ACTs are currently the most effective and widely recommended antimalarial drugs. They combine an artemisinin derivative, which rapidly reduces the parasite load, with a longer-acting partner drug to ensure the complete elimination of the parasites. Common artemisinin derivatives include artemether, artesunate, and dihydroartemisinin.
- Chloroquine: In regions where Plasmodium vivax and Plasmodium ovale are sensitive to chloroquine, this drug may be used. However, chloroquine-resistant strains of Plasmodium falciparum are prevalent in many malaria-endemic areas, limiting its effectiveness against this more severe species.
Treatment guidelines:
- The World Health Organization (WHO) provides guidelines for the treatment of malaria, recommending specific antimalarial regimens based on the local prevalence of drug-resistant strains.
- Prompt and accurate diagnosis is crucial for determining the appropriate treatment regimen.
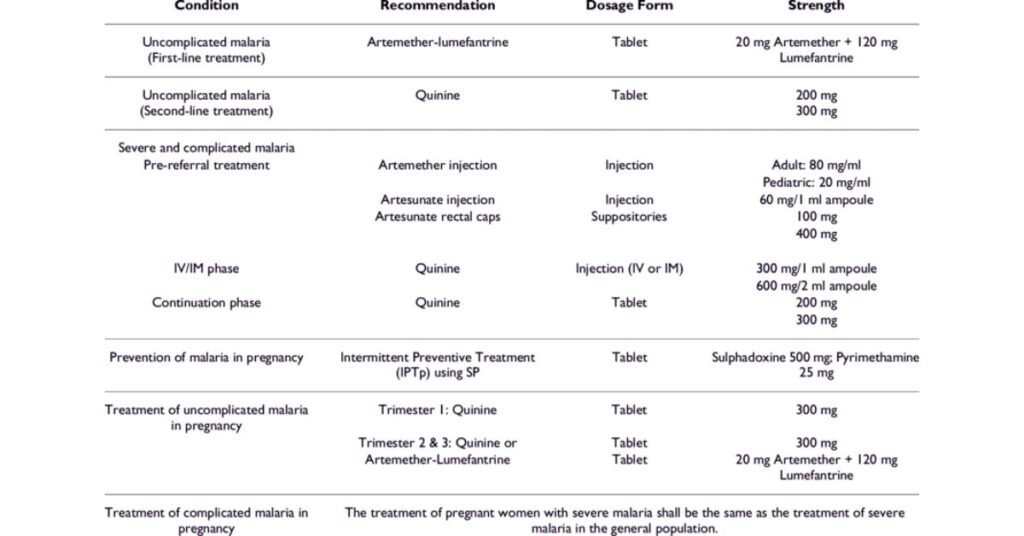
Severe malaria treatment:
- Severe malaria, often caused by Plasmodium falciparum, is a medical emergency that requires immediate attention. In severe cases, treatment may involve intravenous (IV) administration of antimalarial drugs such as artesunate.
- Other supportive measures, including blood transfusions for severe anemia and fluid management, may be necessary in severe cases.
Primaquine for radical cure:
- For the treatment of P. vivax and P. ovale infections, a drug called primaquine is often used to eliminate the dormant liver forms (hypnozoites) and prevent relapses. However, primaquine use requires caution due to the risk of hemolysis in individuals with glucose-6-phosphate dehydrogenase (G6PD) deficiency.
Combination therapies for multidrug resistance:
- In areas with multidrug-resistant malaria, combination therapies involving multiple antimalarial drugs may be used to improve treatment efficacy and reduce the risk of drug resistance development.
Prevention of malaria in high-risk areas:
- In regions where malaria is endemic, preventive measures such as chemoprophylaxis (preventing infection before it occurs) may be recommended for travelers or individuals at high risk of exposure.
Monitoring and follow-up:
- Regular monitoring of patients during treatment is essential to assess the response to medication and detect any potential adverse effects.
- Follow-up care may involve repeated blood tests to confirm parasite clearance and ensure the effectiveness of the chosen treatment.
It’s crucial for healthcare providers to adhere to established treatment guidelines and consider local factors such as drug resistance patterns when determining the most appropriate antimalarial regimen.
What are the complications of malaria?
Malaria, if not promptly and effectively treated, can lead to a range of complications, some of which can be life-threatening. The severity of complications often depends on factors such as the species of the Plasmodium parasite, the patient’s age, and the timeliness of medical intervention.
Severe anemia: Malaria can cause the destruction of red blood cells, leading to anemia. Severe anemia is especially common in children and pregnant women. In some cases, the rapid destruction of red blood cells can overwhelm the body’s ability to compensate, resulting in profound anemia.
Cerebral malaria: Cerebral malaria is a severe and potentially fatal complication, primarily associated with infections caused by Plasmodium falciparum. It occurs when the parasite-infected red blood cells obstruct the blood vessels in the brain, leading to impaired blood flow and potential brain damage. Symptoms may include seizures, altered consciousness, and neurological deficits.
Multi-organ failure: Severe malaria can progress to multi-organ failure, affecting vital organs such as the kidneys, liver, and lungs. Organ failure may result from a combination of factors, including the sequestration of infected red blood cells in the microvasculature and the release of toxic byproducts from the parasite.
Acute respiratory distress syndrome (ARDS): Severe malaria infections, particularly those caused by P. falciparum, can lead to acute respiratory distress syndrome. This condition is characterized by severe respiratory failure, difficulty breathing, and a decrease in blood oxygen levels.
Renal failure: Malaria can affect the kidneys, leading to impaired renal function and, in severe cases, renal failure. The accumulation of waste products in the blood can contribute to metabolic imbalances and further complications.
Hemoglobinuria (Blackwater Fever): Hemoglobinuria, also known as blackwater fever, is a severe complication associated with the breakdown of red blood cells. This can lead to the release of hemoglobin into the bloodstream, causing the urine to turn dark or black. Blackwater fever is more commonly associated with P. falciparum infections.
Pulmonary edema: Severe malaria may result in the accumulation of fluid in the lungs, leading to pulmonary edema. This can further compromise respiratory function and contribute to respiratory distress.
Hypoglycemia: Malaria can cause low blood sugar levels (hypoglycemia), especially in children. Hypoglycemia can lead to seizures, loss of consciousness, and other serious complications.
Pregnancy complications: Pregnant women are at an increased risk of severe malaria and its complications. Malaria during pregnancy can lead to maternal anemia, low birth weight, preterm birth, and an increased risk of infant mortality.
It is crucial to emphasize that complications can develop rapidly, and severe malaria requires immediate medical attention.
How is malaria prevented?
Preventing malaria involves a combination of strategies aimed at reducing human exposure to infected mosquitoes, detecting and treating infections promptly, and implementing measures to control the mosquito vector population. Here’s a detailed overview of key malaria prevention methods:
Vector control:
- Insecticide-treated bed nets (ITNs): Distribution and use of ITNs, which are bed nets treated with long-lasting insecticides, are a highly effective means of preventing mosquito bites during sleep. ITNs create a physical barrier and kill or repel mosquitoes that come into contact with the net.
- Indoor residual spraying (IRS): IRS involves the application of insecticides on the interior walls of houses, reducing the lifespan of mosquitoes that land on treated surfaces. This method is particularly effective in areas with high mosquito populations and indoor feeding behavior.
- Environmental management: Eliminating or modifying mosquito breeding sites, such as stagnant water sources, can reduce mosquito populations. This includes proper waste disposal, clearing blocked drains, and avoiding the accumulation of water in containers.
Chemoprophylaxis: Travelers to malaria-endemic regions may be prescribed prophylactic antimalarial drugs before, during, and after their trip. The choice of medication depends on the destination and the risk of drug resistance in the region.
Intermittent preventive treatment in pregnancy (IPTp): Pregnant women in malaria-endemic areas are often provided with intermittent preventive treatment using antimalarial drugs to reduce the risk of maternal anemia, low birth weight, and other complications associated with malaria during pregnancy.
Chemoprevention for high-risk groups: In some regions, especially in Africa, seasonal malaria chemoprevention is recommended for children under the age of five. This involves the administration of antimalarial drugs during the high-transmission season to prevent malaria episodes.
Early diagnosis and prompt treatment: Timely diagnosis and effective treatment of malaria cases are crucial for preventing the spread of the disease and reducing the risk of severe complications. Diagnostic methods include microscopy, rapid diagnostic tests (RDTs), and molecular techniques.
Community education and empowerment: Informing communities about malaria transmission, prevention methods, and the importance of seeking prompt medical care can empower individuals to take active roles in protecting themselves and their communities.
Vaccination: The development and implementation of malaria vaccines, such as the RTS,S/AS01 (Mosquirix) vaccine, offer an additional tool for preventing malaria. Vaccination efforts are ongoing, and the integration of vaccines into existing prevention strategies is being explored.
It’s important to note that a combination of interventions, known as integrated vector management (IVM), is often the most effective approach to malaria prevention. This involves combining various methods tailored to the local context and the specific characteristics of the malaria transmission cycle. Sustainable and community-based approaches are crucial for the long-term success of malaria prevention efforts.
Takeaway
In conclusion, understanding the comprehensive landscape of malaria, encompassing its causes, symptoms, diagnosis, treatments, complications, and prevention strategies, is paramount for effective public health initiatives. By emphasizing the importance of integrated approaches, including vector control, chemoprophylaxis, and community education, we can collectively work towards not only treating malaria but also preventing its spread and minimizing its potentially devastating impact on vulnerable populations worldwide.
Frequently Asked Questions
Q: What is malaria?
A: Malaria is a tropical disease caused by the Plasmodium parasite, transmitted to humans through the bite of infected female Anopheles mosquitoes.
Q: What are the common symptoms of malaria?
A: Symptoms include fever, chills, sweating, headache, muscle aches, and fatigue. In severe cases, it can lead to organ failure and death.
Q: How is malaria diagnosed?
A: Diagnosis involves blood tests to detect the presence of the Plasmodium parasite. Rapid diagnostic tests and microscopy are commonly used methods.
Q: Where is malaria most prevalent?
A: Malaria is most prevalent in tropical and subtropical regions, particularly in sub-Saharan Africa, Southeast Asia, and parts of Central and South America.
Q: Can malaria be prevented?
A: Yes, malaria can be prevented through the use of bed nets, insect repellents, antimalarial drugs, and environmental control measures to reduce mosquito breeding.
Q: How is malaria treated?
A: Malaria is treated with antimalarial medications. The choice of medication depends on the type of Plasmodium parasite causing the infection and the severity of the disease.
Q: Is there a vaccine for malaria?
A: Yes, a malaria vaccine called RTS,S has been developed and is being used in some regions to help prevent the disease, although its effectiveness varies.
Q: Can malaria be transmitted from person to person?
A: Malaria is not directly transmitted from person to person. It requires the involvement of mosquitoes in the transmission cycle.
Q: How can travelers protect themselves from malaria?
A: Travelers to malaria-endemic areas should take antimalarial prophylaxis, use insect repellents, sleep under bed nets, and take other preventive measures.
Q: What is drug resistance in the context of malaria?
A: Drug resistance occurs when the Plasmodium parasites evolve to withstand the effects of antimalarial drugs, making treatment less effective. Monitoring and managing drug resistance are crucial aspects of malaria control.
Q: Are pregnant women more susceptible to malaria?
A: Yes, pregnant women are at an increased risk of malaria complications. It can lead to maternal anemia, low birth weight, and other adverse outcomes. Malaria prevention and treatment are especially important for pregnant women.
Q: How is malaria research contributing to control and prevention efforts?
A: Ongoing research focuses on developing new drugs, understanding mosquito behavior, and improving vaccine efficacy. Research plays a crucial role in advancing malaria control and prevention strategies.
References
- World Health Organization (WHO). (2022). Malaria Fact Sheet. https://www.who.int/news-room/fact-sheets/detail/malaria
- Centers for Disease Control and Prevention (CDC). (2022). Malaria – About Malaria. https://www.cdc.gov/malaria/about/index.html
- Ashley, E. A., & White, N. J. (2014). The duration of Plasmodium falciparum infections. Malaria Journal, 13(1), 500. https://malariajournal.biomedcentral.com/articles/10.1186/1475-2875-13-500
- Ashley, E. A., Dhorda, M., Fairhurst, R. M., Amaratunga, C., Lim, P., Suon, S., … & Hien, T. T. (2014). Spread of artemisinin resistance in Plasmodium falciparum malaria. New England Journal of Medicine, 371(5), 411-423. https://www.nejm.org/doi/full/10.1056/NEJMoa1314981