Types | Risks | Symptoms | Diagnosis | Treatment | Complications | Prevention | Takeaway | FAQs
The history of influenza is a tale of pandemics, with the most notorious being the 1918 Spanish flu, which claimed millions of lives worldwide. We will explore how the understanding and management of influenza have evolved over the years.
What is influenza (Flu)?
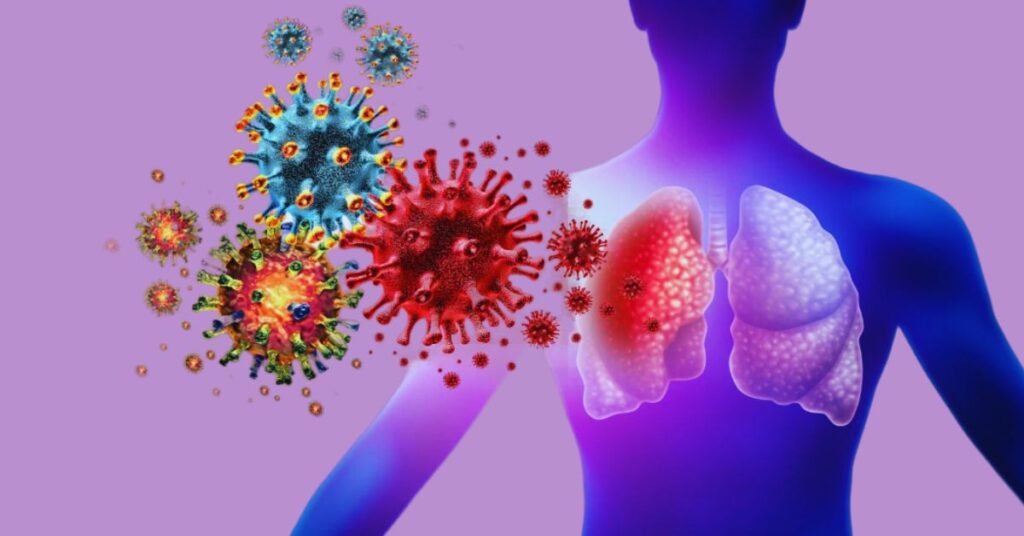
Influenza, or simply the flu, is a highly contagious viral infection that primarily affects the respiratory system. It is caused by influenza viruses, primarily belonging to the Orthomyxoviridae family, and is known for its ability to cause seasonal epidemics and occasional pandemics. The flu can vary in severity, from mild to severe, and it can lead to hospitalizations and, in some cases, fatalities, particularly among vulnerable populations such as the elderly, young children, and individuals with weakened immune systems.
What are the types of influenza (Flu)?
Influenza is not a single disease but a group of related respiratory illnesses caused by influenza viruses. These viruses are classified into three main types: Influenza A, Influenza B, and Influenza C. Each type has its own unique characteristics and plays a distinct role in the annual occurrence of flu outbreaks.
Influenza A
Structure: Influenza A viruses are characterized by their genetic diversity and are the most virulent and adaptable of the three types. They have an outer envelope containing two key surface proteins, hemagglutinin (H) and neuraminidase (N), which are used to classify subtypes. There are 18 different H subtypes and 11 different N subtypes, creating a multitude of possible combinations. For example, you may have heard of H1N1 or H3N2 – these represent specific subtypes of Influenza A.
Variability: Influenza A viruses have a high mutation rate, which allows them to quickly adapt to new hosts and environments. This is why they are often associated with seasonal epidemics and occasional pandemics. Pandemics, such as the 1918 Spanish flu, 1957 Asian flu, and 2009 H1N1 pandemic, are typically caused by significant changes in the H and N subtypes.
Host Range: Influenza A viruses have a broad host range, capable of infecting birds, humans, pigs, and other animals. Avian influenza, or bird flu, is a well-known example of a subtype of Influenza A that primarily infects birds but can occasionally jump to humans.
Influenza B
Structure: Influenza B viruses have a more stable genome than Influenza A and do not have the same range of subtypes. They are classified into two distinct lineages: Victoria and Yamagata.
Variability: Influenza B viruses undergo slower antigenic changes compared to Influenza A, making them less likely to cause pandemics. However, they are responsible for seasonal outbreaks and can still result in severe illness.
Host Range: Influenza B primarily infects humans and does not have the same zoonotic potential as Influenza A, which means it is less likely to jump from animals to humans.
Influenza C
Structure: Influenza C viruses are structurally different from Influenza A and B, lacking the H and N proteins. Instead, they have hemagglutinin-esterase-fusion (HEF) protein on their surface. Influenza C is less common and typically causes mild respiratory symptoms.
Variability: Influenza C is relatively stable and does not undergo significant changes like Influenza A or B, which is why it doesn’t lead to large-scale seasonal epidemics.
Host Range: Influenza C primarily infects humans and, to a lesser extent, pigs and dogs. It is not associated with pandemics.
How is influenza (Flu) transmitted?
The influenza virus is highly transmissible and disseminates via respiratory droplets when an afflicted individual coughs or sneezes.
Close contact: The virus is most commonly spread when an infected person coughs, sneezes, or talks. Respiratory droplets containing the virus can be inhaled by individuals nearby.
Contaminated surfaces: Influenza viruses can survive on surfaces for a limited period. If a person touches a contaminated surface and then touches their mouth, nose, or eyes, they can introduce the virus into their respiratory tract.
Airborne transmission: In certain situations, particularly in enclosed spaces, the virus can remain suspended in the air and infect people who breathe in these airborne particles.
Seasonal causes
The flu exhibits a seasonal pattern in many parts of the world, typically peaking in the winter months. Several factors contribute to this seasonality:
- Cold weather: In colder climates, people tend to spend more time indoors in close proximity, increasing the chances of virus transmission.
- Low humidity: Dry indoor air during the winter can lead to drier respiratory mucosa, making it easier for the virus to enter the body.
- Holiday travel: Increased travel and gatherings during the holiday season can facilitate the spread of the virus.
Pandemic causes
Pandemics, which are global outbreaks of a new strain of influenza, are caused by significant changes in the influenza A virus. These changes can result from:
- Antigenic shift: This occurs when two different influenza A viruses infect a host, leading to a reassortment of their genetic material. This can create a new subtype to which humans have little to no immunity, causing a pandemic.
- Zoonotic transmission: When an animal influenza virus, such as avian influenza (bird flu) or swine influenza, jumps to humans, it can lead to a pandemic if it is highly transmissible and causes severe disease.
What are the symptoms of influenza (Flu)?
Influenza is characterized by a range of symptoms that can vary in severity from mild to severe.

The common symptoms of influenza include:
- Fever: One of the hallmark symptoms of the flu is a sudden and often high fever, typically above 100.4°F (38°C). Fever is a response to the infection and is usually accompanied by chills.
- Cough: A dry, persistent cough. This cough can be quite bothersome and may lead to a sore throat.
- Sore throat: Influenza can cause a scratchy or painful throat, making it uncomfortable to swallow or talk.
- Runny or stuffy nose: Many people with the flu experience nasal congestion, with a runny or stuffy nose. This can be accompanied by sneezing and sinus discomfort.
- Fatigue: Profound fatigue and weakness are common flu symptoms. You may feel extremely tired and lack energy, which can be disabling.
- Muscle aches (Myalgia): Muscle aches and joint pain are frequent symptoms of the flu, often affecting large muscle groups. This can make even simple movements uncomfortable.
- Headache: Headaches are a common symptom of the flu and are typically characterized by a throbbing or pounding sensation.
- Body aches (Malaise): Generalized body aches and a feeling of overall discomfort, known as malaise, are common during a flu infection.
- Respiratory symptoms: Some individuals with the flu may develop respiratory symptoms such as shortness of breath and chest discomfort. In severe cases, pneumonia can develop.
- Gastrointestinal symptoms: While less common, some people with the flu may experience gastrointestinal symptoms, including nausea, vomiting, and diarrhea.
- Loss of appetite: A reduced or complete loss of appetite is another potential flu symptom. Dehydration can be a concern if you’re not eating or drinking.
- High fever in children: In young children, the flu can sometimes lead to very high fevers, seizures, and febrile convulsions. It’s important to monitor children closely and seek medical attention if their fever is extremely high.
Influenza symptoms often come on suddenly, and they can make individuals feel extremely unwell, sometimes requiring bed rest. While many cases of the flu resolve on their own with rest and supportive care, severe cases or those in high-risk individuals, such as the very young, the elderly, and those with weakened immune systems, can lead to complications like pneumonia and hospitalization.
How is influenza (Flu) diagnosed?
Diagnosing influenza involves a combination of clinical evaluation, patient history, and laboratory tests. The diagnosis is crucial for appropriate management and treatment.
Clinical evaluation:
- Medical history: Healthcare professionals begin the diagnostic process by taking a detailed medical history. They will ask questions about the patient’s symptoms, their onset, and any recent exposure to individuals with the flu.
- Physical examination: A thorough physical examination may be conducted to assess the patient’s general health and specific symptoms. The healthcare provider will check for signs like fever, cough, and any respiratory distress.
Rapid influenza diagnostic tests (RIDTS):
Rapid influenza diagnostic tests, or RIDTS, are a common method for diagnosing influenza. These tests can provide results within 15-30 minutes and are often performed in a healthcare provider’s office or clinic. The procedure involves:
- Nasal or throat swab: A swab is taken from the patient’s nasal or throat secretions.
- Test kit: The swab sample is placed in a test kit that contains antibodies specifically designed to detect influenza A and B viruses.
- Results: A positive result indicates the presence of the influenza virus, while a negative result suggests the absence of the virus. However, ridts may have limitations in terms of sensitivity and specificity, and false negatives can occur.
Reverse transcription polymerase chain reaction (RT-PCR):
RT-PCR is a highly sensitive and specific laboratory test that can accurately diagnose influenza. It is often used to confirm the diagnosis in cases of severe illness or when rapid test results are inconclusive. The RT-PCR process involves:
- Sample collection: A nasal or throat swab is taken, similar to RIDTS.
- RNA extraction: The genetic material (RNA) of the virus is extracted from the collected sample.
- Amplification: The viral RNA is amplified using a polymerase chain reaction, which can detect even small amounts of the virus.
- Detection: The test can differentiate between influenza A and B viruses and provide a positive or negative result.
Viral culture:
Viral culture is a less common but highly specific method for diagnosing influenza. It involves:
- Sample collection: A sample is collected through a nasal or throat swab.
- Culturing: The collected sample is placed in a laboratory dish with cells that can support the growth of the influenza virus.
- Observation: If the virus grows in the culture, it can be identified and confirmed as the influenza virus.
Serological testing:
Serological tests involve analyzing blood samples to detect the presence of antibodies produced by the immune system in response to an influenza infection. These tests can be used to determine if an individual has been exposed to the virus and has developed immunity. However, they are not commonly used for diagnosing acute cases of influenza.
Chest X-rays and other imaging:
In some cases, especially when the flu leads to complications like pneumonia, chest X-rays or other imaging studies may be performed to evaluate the condition of the lungs.
The choice of diagnostic method depends on the clinical presentation and the need for rapid results or confirmation. Accurate diagnosis is essential for effective management and treatment of the flu, as well as for public health surveillance during flu outbreaks.
What’s the treatment for influenza (Flu)?
The treatment of influenza is primarily supportive and aimed at relieving symptoms, as it is a self-limiting condition in most cases.
Supportive care
Supportive care is the cornerstone of influenza treatment and involves various measures to alleviate symptoms and promote recovery:
- Rest: Adequate rest is crucial for the body to fight off the infection. It helps conserve energy and allows the immune system to work more effectively.
- Hydration: Staying well-hydrated is essential, especially if there is a fever, as it helps reduce the risk of dehydration. Clear fluids like water, herbal teas, and broths can help.
- Fever management: Over-the-counter fever-reducing medications like acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) can help lower fever and relieve body aches. Aspirin should be avoided in children and teenagers with the flu due to the risk of Reye’s syndrome, a rare but serious condition.
- Cough suppressants and expectorants: Over-the-counter medications may provide relief for a persistent cough. Cough suppressants can help reduce the urge to cough, while expectorants may help loosen mucus if you have a productive cough.
- Throat lozenges: Sore throat can be soothed with throat lozenges or warm saltwater gargles.
Antiviral medications:
Antiviral medications can be prescribed for the treatment of influenza, especially in the following situations:
- High-risk groups: Individuals at high risk of developing complications from the flu, such as the elderly, very young children, pregnant women, individuals with underlying medical conditions (e.g., asthma, diabetes, heart disease), and immunocompromised individuals, are more likely to benefit from antiviral treatment.
- Early treatment: Antiviral drugs are most effective when administered early in the course of the illness, ideally within the first 48 hours after symptom onset. They can reduce the severity and duration of symptoms and may prevent complications.
- Severe cases: For individuals with severe influenza, especially those with complications like pneumonia, antiviral treatment may be essential. Hospitalized patients with influenza are often given antiviral medications.
The two main antiviral drugs used to treat influenza are:
- Oseltamivir (Tamiflu): This is available in both oral and suspension forms and is approved for use in adults and children over 2 weeks old.
- Zanamivir (Relenza): This is administered through an inhaler and is approved for individuals aged 7 and older.
Isolation and hygiene:
To prevent the spread of influenza, individuals with the flu should:
- Stay home: Infected individuals should stay home until they are fever-free for at least 24 hours without the use of fever-reducing medications.
- Practice respiratory hygiene: Covering the mouth and nose when coughing or sneezing with a tissue or elbow can help prevent the spread of the virus to others.
What are the complications of influenza (Flu)?
Influenza can lead to various complications, especially in vulnerable populations. These complications can range from mild to severe and require medical attention.
Secondary bacterial infections:
One of the most common and concerning complications of the flu is the development of secondary bacterial infections. Influenza can weaken the immune system and damage the respiratory tract, making individuals more susceptible to bacterial infections. Common bacterial infections that may follow the flu include:
- Pneumonia: Bacterial pneumonia is a serious and potentially life-threatening complication. It can lead to severe respiratory distress and may require hospitalization.
- Ear Infections: The flu can lead to middle ear infections, particularly in children.
- Sinus Infections: Influenza can increase the risk of sinusitis, characterized by pain and inflammation in the sinuses.
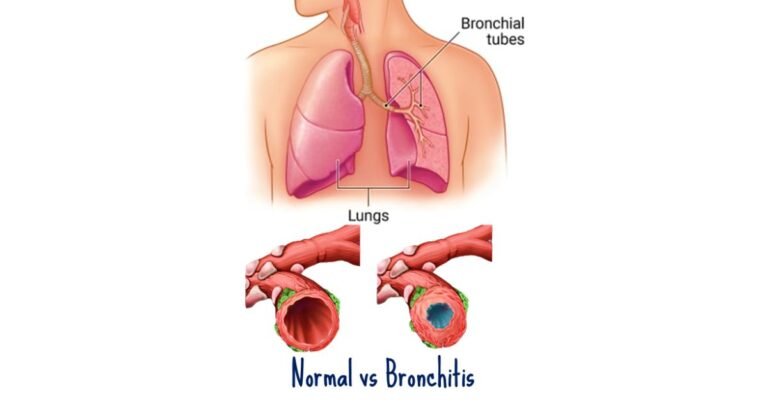
- Bronchitis: Acute bacterial bronchitis can develop in some cases, causing persistent cough and chest discomfort.
Exacerbation of chronic medical conditions:
Individuals with underlying health conditions, such as asthma, chronic obstructive pulmonary disease (COPD), heart disease, diabetes, or a weakened immune system, are at a higher risk of experiencing a worsening of their condition during and after an influenza infection. The flu can exacerbate these chronic conditions, leading to hospitalization or even death in some cases.
Neurological complications:
In rare instances, the flu can lead to neurological complications, particularly in children. These complications may include:
- Encephalitis: Inflammation of the brain can result in seizures, confusion, and neurological deficits.
- Reye’s syndrome: Although extremely rare, Reye’s syndrome is a severe condition that can affect the brain and liver. It is associated with aspirin use in children with the flu and can lead to liver failure and neurological damage.
Cardiac complications:
The flu can increase the risk of cardiac events, particularly in individuals with pre-existing heart conditions. Cardiac complications may include:
- Myocarditis: Inflammation of the heart muscle can lead to chest pain, arrhythmias, and heart failure.
- Pericarditis: Inflammation of the lining around the heart can result in chest pain and discomfort.
Hospitalization and death:
Severe complications of the flu can lead to hospitalization, and in the most severe cases, death. Vulnerable populations, including the very young, the elderly, pregnant women, and those with weakened immune systems or chronic medical conditions, are at a higher risk of experiencing these severe outcomes.
Dehydration:
Fever, sweating, and decreased fluid intake due to flu symptoms can lead to dehydration, especially in children and the elderly. Dehydration can worsen overall health and lead to complications like kidney problems and electrolyte imbalances.
How is influenza (Flu) prevented?
Preventing influenza is essential to reduce the risk of infection, complications, and the burden on healthcare systems.
Influenza vaccination
Annual influenza vaccination is the most effective way to prevent the flu. The flu vaccine is designed to protect against the strains of the virus expected to be most prevalent during the upcoming flu season. Key points regarding influenza vaccination include:
Who should get vaccinated?
Nearly everyone over the age of six months is recommended to receive the influenza vaccine. Specific focus is given to individuals at high risk of complications, such as the elderly, young children, pregnant women, and those with chronic medical conditions.
Timing:
Influenza vaccination is typically available in the early fall before the flu season begins. It is recommended to get vaccinated before the flu is circulating widely in the community to ensure the highest level of protection.
Vaccine effectiveness:
While the effectiveness of the flu vaccine can vary from year to year, it remains the best defense against the virus. Even if it doesn’t prevent the flu entirely, it can reduce the severity of symptoms and the risk of complications.
Good hygiene practices
Practicing good hygiene can help prevent the spread of the flu:
- Handwashing: Regularly washing hands with soap and water for at least 20 seconds is crucial. Hand sanitizer with at least 60% alcohol can also be used when soap and water are not available.
- Respiratory etiquette: Covering the mouth and nose with a tissue or elbow when coughing or sneezing can help prevent respiratory droplets from spreading the virus.
- Avoiding touching the face: Touching the eyes, nose, and mouth with unwashed hands can introduce the virus into the body.
Avoiding close contact
Minimizing close contact with individuals who have the flu can reduce the risk of transmission. Individuals who are sick with the flu should stay home to prevent the spread of the virus to others.
Face masks
During flu outbreaks, the use of face masks, particularly in healthcare settings, can help prevent the spread of the virus. N95 respirators are highly effective in filtering out small particles and can provide protection for healthcare workers and individuals in close contact with flu patients.
High-risk groups
Particular attention should be given to individuals at high risk of complications from the flu. Recommendations for these groups may include:
- Vaccination: High-risk individuals should receive the flu vaccine every year.
- Prophylactic antivirals: In some cases, especially during outbreaks, antiviral medications may be prescribed as a preventive measure.
- Isolation: High-risk individuals who have been exposed to the flu should avoid contact with infected individuals.
Public health measures
Public health agencies play a crucial role in influenza prevention:
- Surveillance: Monitoring flu activity and identifying circulating strains to inform vaccine development.
- Vaccination programs: Implementing vaccination campaigns to reach the maximum number of people.
- Education: Providing information to the public about flu prevention and the importance of vaccination.
- Quarantine and isolation: In outbreak situations, public health measures like quarantine and isolation may be necessary to limit the spread of the virus.
Influenza prevention involves a combination of vaccination, good hygiene practices, and public health measures. Public health efforts play a significant role in tracking and managing flu outbreaks. By taking these preventive steps, individuals and communities can reduce the impact of the flu on public health and well-being.
Takeaway
Influenza (Flu) is a viral infection that can affect anyone, but with proper prevention, early diagnosis, and suitable treatment, the impact can be minimized. Remember, getting a flu shot, maintaining good hygiene, and seeking medical attention when needed are your best defenses against the flu.
Frequently Asked Questions
Q: Can I get the flu from the flu vaccine?
A: No, the flu vaccine contains inactivated or weakened viruses and cannot cause the flu.
Q: How long does the flu typically last?
A: The flu usually lasts 1 to 2 weeks, with symptoms being most severe during the first few days.
Q: Who is at high risk for flu complications?
A: Children, the elderly, pregnant women, and individuals with certain underlying health conditions are more susceptible to severe flu-related complications.
Q: Can you get the flu from touching an infected surface?
A: Yes, the virus can survive on surfaces for a short period, so it’s important to practice good hand hygiene.
Q: Is it safe to get a flu shot during pregnancy?
A: Yes, flu vaccination during pregnancy is safe and highly recommended to protect both the mother and the baby.
Q: Can antibiotics treat the flu?
A: No, antibiotics are ineffective against viral infections like the flu.
References
- Paules, C. I., Marston, H. D., & Eisinger, R. W. (2017). Influenza: The once and future pandemic. Clinical Microbiology Reviews, 30(1), 1-28.
- Jester, B. J., Uyeki, T. M., & Jernigan, D. B. (2019). Readiness for responding to a severe pandemic 100 years after 1918. American Journal of Epidemiology, 188(3), 489-492.
- Centers for Disease Control and Prevention (CDC). (2022). Influenza (Flu). https://www.cdc.gov/flu/index.htm
- World Health Organization (WHO). (2022). Influenza (Seasonal). https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal)
- National Institute of Allergy and Infectious Diseases (NIAID). (2022). Influenza (Flu). https://www.niaid.nih.gov/diseases-conditions/influenza