Types | Transmission | Symptoms | Diagnosis | Treatment | Complications | Prevention | Takeaway | FAQs
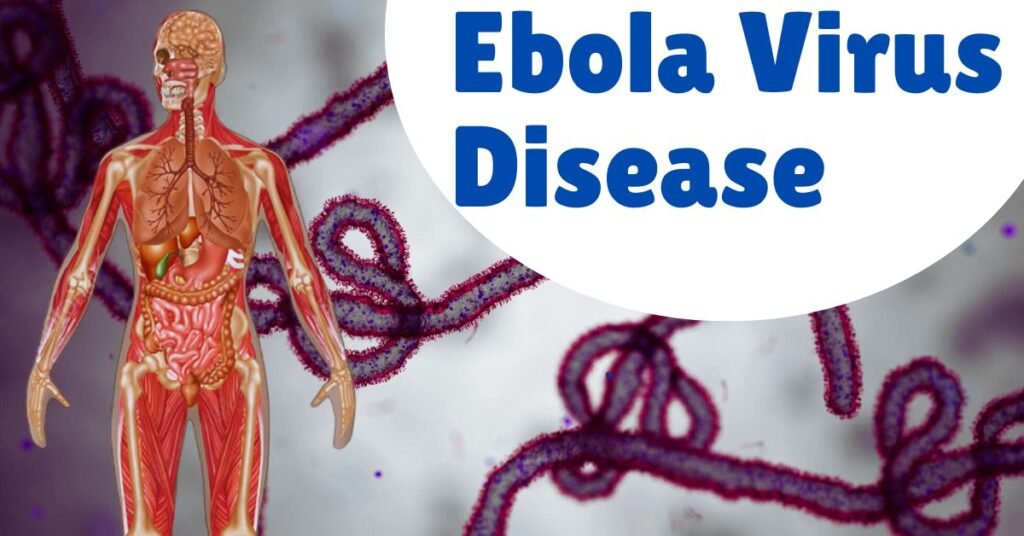
Ebola virus disease is a severe illness that can lead to death in humans. It is characterized by symptoms such as fever, severe headache, muscle pain, weakness, fatigue, diarrhea, vomiting, abdominal pain, and unexplained bleeding or bruising.
What is Ebola virus disease?
Ebola virus disease (EVD), also known as Ebola hemorrhagic fever, is a severe and often fatal illness in humans. It is caused by infection with the Ebola virus, which belongs to the family Filoviridae. EVD was first identified in 1976 during simultaneous outbreaks in Nzara, South Sudan, and Yambuku, Democratic Republic of Congo (formerly Zaire), with the latter outbreak occurring near the Ebola River, from which the disease takes its name.
What are the types of Ebola virus disease?
There are several known types, or species, of the Ebola virus, each with distinct characteristics and varying degrees of virulence. The following are the recognized types of Ebola virus:
Zaire ebolavirus (EBOV):
- This is the most virulent strain of Ebola virus, with the highest mortality rate recorded among all Ebola outbreaks.
- It was first identified in 1976 in what is now the Democratic Republic of the Congo (formerly Zaire), near the Ebola River, from which it derives its name.
- Outbreaks of Zaire ebolavirus have occurred predominantly in Central Africa, including recent outbreaks in the Democratic Republic of the Congo and outbreaks in West Africa in 2014-2016.
Sudan ebolavirus (SUDV):
- Sudan ebolavirus was first identified in 1976, coinciding with the discovery of Zaire ebolavirus, during an outbreak in Sudan (now South Sudan).
- It is less virulent than Zaire ebolavirus but still causes severe illness and has a high mortality rate.
- Outbreaks of Sudan ebolavirus have occurred in several African countries, including South Sudan, Uganda, and the Democratic Republic of the Congo.
Taï Forest ebolavirus (TAFV):
- Taï Forest ebolavirus was first identified in 1994 when it caused an outbreak among chimpanzees in the Taï Forest in Côte d’Ivoire.
- It is named after the location of its discovery.
- TAFV has only caused a single known human case, which occurred in a researcher who conducted an autopsy on an infected chimpanzee.
Bundibugyo ebolavirus (BDBV):
- Bundibugyo ebolavirus was first identified in 2007 in an outbreak in the Bundibugyo District of Uganda.
- It is less common than Zaire and Sudan ebolaviruses but can still cause severe illness with a significant mortality rate.
- Outbreaks of Bundibugyo ebolavirus have been reported in Uganda and the Democratic Republic of the Congo.
Reston ebolavirus (RESTV):
- Reston ebolavirus was first discovered in 1989 when it caused an outbreak among monkeys imported from the Philippines to Reston, Virginia, USA.
- It is the only Ebola virus species that has not caused illness in humans, although it has led to severe illness in non-human primates.
- RESTV has been found in the Philippines and China, where it has caused outbreaks among pigs.
These five types of Ebola virus differ in their geographic distribution, virulence, and potential for causing outbreaks. While some, like Zaire and Sudan ebolaviruses, have caused devastating outbreaks with high mortality rates, others, like Taï Forest ebolavirus, have been less prevalent in human populations.
How does Ebola virus disease spread?
Ebola virus disease (EVD) spreads primarily through direct contact with the bodily fluids of infected individuals or animals. The Ebola virus is highly contagious and can be transmitted through various means:
- Direct contact: The most common mode of transmission is through direct contact with blood, saliva, vomit, urine, feces, sweat, semen, or other bodily fluids of infected individuals. This can occur through activities such as caring for the sick, touching contaminated surfaces or objects, or participating in traditional burial practices that involve close contact with the deceased.
- Indirect contact: Ebola virus can also spread indirectly through contact with objects or surfaces contaminated with the virus. For example, touching surfaces or medical equipment contaminated with infected bodily fluids can lead to transmission if proper hygiene practices are not observed.
- Airborne transmission: Although Ebola virus is not typically considered airborne, there is evidence to suggest that the virus may be transmitted through aerosolized droplets under certain conditions. This can occur in healthcare settings during medical procedures that generate aerosols, such as intubation or suctioning, increasing the risk of transmission to healthcare workers.
- Transmission from animals: Ebola virus can be transmitted to humans through contact with infected animals, particularly fruit bats and primates (such as apes and monkeys) that serve as natural hosts for the virus. Handling or consuming bushmeat (wild animals hunted for food) can lead to transmission if the animals are infected with the virus.
- Sexual transmission: Ebola virus can be transmitted through sexual contact with survivors of EVD, even after they have recovered from the illness. The virus can persist in semen for months after recovery, posing a risk of sexual transmission to partners.
- Healthcare settings: Healthcare workers are at high risk of contracting Ebola virus disease due to their close contact with infected patients and exposure to contaminated materials. Inadequate infection control measures, such as improper use of personal protective equipment or unsafe handling of medical waste, can contribute to transmission within healthcare settings.
Once the Ebola virus enters the human body, it targets various cells of the immune system, leading to widespread systemic infection. The virus replicates rapidly, causing damage to blood vessels, organs, and the immune system. This can result in a range of symptoms, including fever, severe headache, muscle pain, weakness, fatigue, diarrhea, vomiting, abdominal pain, and unexplained bleeding or bruising.
What are the symptoms of Ebola virus disease?
The symptoms of EVD can vary widely in severity and may mimic those of other infectious diseases, making diagnosis challenging. However, there are several hallmark symptoms associated with Ebola virus infection:
- Fever: Fever is one of the earliest and most common symptoms of Ebola virus disease. Patients typically experience a sudden onset of high fever, often exceeding 38.6°C (101.5°F). Fever is usually accompanied by chills and sweating.
- Headache: Severe headache is another prominent symptom of EVD. Patients often describe the headache as intense and persistent, sometimes leading to photophobia (sensitivity to light) and difficulty concentrating.
- Muscle pain and weakness: Ebola virus infection can cause severe muscle pain, joint pain, and general weakness throughout the body. Patients may experience fatigue and difficulty performing daily activities due to muscle weakness.
- Gastrointestinal symptoms: Ebola virus disease commonly presents with gastrointestinal symptoms such as abdominal pain, nausea, vomiting, and diarrhea. Diarrhea may be profuse and watery, leading to dehydration and electrolyte imbalances.
- Unexplained bleeding: Some patients with EVD may develop bleeding symptoms, although this is not always present. Unexplained bleeding may manifest as blood in the stool, vomit, or urine, as well as bleeding from the gums, nose, or injection sites. However, bleeding is relatively uncommon in Ebola cases compared to other symptoms.
- Rash: A maculopapular rash may develop in some patients with EVD, typically appearing around 5 to 7 days after the onset of symptoms. The rash is characterized by small, raised bumps on the skin that may be itchy or painful.
- Other symptoms: Additional symptoms of Ebola virus disease may include sore throat, difficulty swallowing, chest pain, shortness of breath, hiccups, confusion, delirium, and neurological symptoms such as seizures or coma in severe cases.
It’s important to note that the severity and combination of symptoms can vary among individuals, and not all patients will experience every symptom.
How is Ebola virus disease diagnosed?
Diagnosing Ebola virus disease (EVD) requires a combination of clinical assessment, laboratory testing, and epidemiological investigation due to the severity and potential public health implications of the disease.
Clinical assessment:
- Healthcare providers first evaluate patients presenting with symptoms consistent with EVD, such as fever, headache, muscle pain, vomiting, diarrhea, and unexplained bleeding.
- A thorough medical history is obtained, including travel history to regions where Ebola virus transmission is known to occur and any potential exposure to infected individuals or animals.
Initial screening:
- Patients suspected of having EVD undergo initial screening to assess their risk of infection based on symptoms, travel history, and exposure to Ebola virus.
- Healthcare providers may use standardized screening tools and questionnaires to identify individuals at high risk of EVD.
Laboratory testing:
- Laboratory testing is essential for confirming the diagnosis of EVD and ruling out other infectious diseases with similar symptoms.
- Blood samples are collected from suspected cases and tested for the presence of Ebola virus genetic material (RNA) using molecular diagnostic techniques such as reverse transcription-polymerase chain reaction (RT-PCR).
- Additional laboratory tests may be performed to assess liver and kidney function, electrolyte levels, coagulation parameters, and other markers of disease severity.
Point-of-care testing:
- In settings with limited laboratory infrastructure, rapid diagnostic tests (RDTs) for Ebola virus may be used for initial screening and triage of suspected cases.
- These tests detect viral antigens or antibodies in blood or other bodily fluids and provide rapid results within a few hours.
Differential diagnosis:
- Positive laboratory test results for Ebola virus RNA confirm the diagnosis of EVD. However, false-positive and false-negative results are possible, so confirmation by repeat testing and validation is necessary.
- Healthcare providers also consider differential diagnoses, including other infectious diseases such as malaria, typhoid fever, influenza, and Lassa fever, which may present with similar symptoms.
Epidemiological investigation:
- Epidemiological investigation plays a crucial role in EVD diagnosis, particularly in outbreak settings.
- Contact tracing and surveillance efforts are conducted to identify and monitor individuals who may have been exposed to the virus, allowing for early detection of additional cases and implementation of control measures.
Specialized laboratory support:
- In outbreaks or complex cases, specialized laboratory support from reference laboratories and public health agencies may be required for confirmatory testing, genomic sequencing, and surveillance activities.
Early diagnosis and prompt isolation of suspected cases are critical for preventing the spread of Ebola virus disease within communities and healthcare settings.
How is Ebola virus disease treated?
Treatment for Ebola virus disease (EVD) primarily focuses on supportive care to manage symptoms, prevent complications, and improve the patient’s chances of survival. As of now, there is no specific antiviral treatment or cure for Ebola virus infection. However, several supportive measures and experimental treatments are used to address the symptoms and complications associated with the disease:
Fluid and electrolyte replacement:
- Patients with EVD often experience severe dehydration due to vomiting, diarrhea, and fluid loss. Intravenous fluids and electrolyte solutions are administered to maintain hydration and electrolyte balance.
- Oral rehydration therapy may be used for patients with mild to moderate dehydration who can tolerate oral fluids.
Management of fever and pain:
- Antipyretic medications such as acetaminophen (paracetamol) may be given to reduce fever and alleviate discomfort.
- Analgesic medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids may be prescribed to manage headache, muscle pain, and other symptoms.
Nutritional support:
- Adequate nutrition is essential for supporting the patient’s immune system and promoting recovery. Nutritional supplements and high-calorie foods may be provided to meet the patient’s energy and nutrient requirements.
Treatment of complications:
- Patients with EVD may develop complications such as coagulation disorders, organ failure, and electrolyte imbalances. Treatment strategies may include blood transfusions, dialysis, mechanical ventilation, and supportive care in intensive care units (ICUs).
Experimental therapies:
- Several experimental treatments have been evaluated for the treatment of Ebola virus disease, including antiviral drugs, monoclonal antibodies, and convalescent plasma therapy.
- Antiviral drugs such as remdesivir have shown promise in preclinical studies and clinical trials for reducing viral replication and improving outcomes in patients with EVD.
- Monoclonal antibodies, such as REGN-EB3 and mAb114, have demonstrated efficacy in reducing mortality rates among patients with Ebola virus infection.
- Convalescent plasma therapy involves transfusing plasma from recovered Ebola patients containing antibodies against the virus into newly infected patients. While this approach has been used in some outbreaks, its efficacy remains uncertain.
Psychosocial support:
- Patients with EVD and their families may experience significant psychological distress due to the severity of the illness and the stigma associated with Ebola virus infection. Psychosocial support services, including counseling and mental health interventions, are important for addressing emotional and social needs during and after treatment.
It’s important to note that the effectiveness of treatment strategies for Ebola virus disease may vary depending on factors such as the patient’s overall health, the timing of treatment initiation, and the availability of medical resources.
What are the complications of Ebola virus disease?
Ebola virus disease (EVD) can lead to a range of complications, some of which can be severe and life-threatening. The complications of EVD can affect multiple organ systems and may result from the direct effects of the virus, as well as the body’s immune response to infection.
Organ failure:
- Ebola virus can cause damage to various organs, including the liver, kidneys, and lungs. Severe systemic inflammation and vascular damage can lead to organ dysfunction and failure.
- Hepatic dysfunction may manifest as elevated liver enzymes, jaundice, and coagulopathy (abnormal blood clotting).
- Renal failure may occur due to acute tubular necrosis and impaired kidney function.
- Respiratory failure can develop in severe cases, leading to acute respiratory distress syndrome (ARDS) and the need for mechanical ventilation.
Hemorrhagic complications:
- Although bleeding is relatively uncommon in Ebola virus disease, some patients may experience hemorrhagic manifestations, including mucosal bleeding, petechiae (small red or purple spots on the skin), and gastrointestinal bleeding.
- Disseminated intravascular coagulation (DIC), a condition characterized by widespread activation of the blood clotting cascade, can lead to both bleeding and thrombotic complications.
Dehydration and electrolyte imbalance:
- Profuse vomiting, diarrhea, and fever can lead to significant fluid and electrolyte losses, resulting in dehydration, electrolyte imbalances, and metabolic abnormalities.
- Hypovolemic shock may develop in severe cases, characterized by inadequate tissue perfusion and oxygen delivery due to decreased blood volume.
Neurological complications:
- Ebola virus can affect the central nervous system, leading to neurological symptoms such as confusion, delirium, seizures, and coma.
- Encephalitis (inflammation of the brain) and meningitis (inflammation of the meninges) may occur in some patients, contributing to neurological complications.
Secondary infections:
- Patients with EVD are susceptible to secondary bacterial and viral infections due to immunosuppression and disruption of the body’s natural defenses.
- Pneumonia, sepsis, urinary tract infections, and skin and soft tissue infections are common complications that can worsen the patient’s condition and increase the risk of mortality.
Psychological and social consequences:
- Survivors of Ebola virus disease may experience long-term psychological and social consequences, including post-traumatic stress disorder (PTSD), depression, anxiety, and stigmatization.
- The social and economic impact of EVD outbreaks can be profound, leading to disruptions in healthcare systems, loss of livelihoods, and community mistrust.
Reproductive complications:
- Ebola virus can persist in semen for several months after recovery from EVD, posing a risk of sexual transmission to partners and potential complications in pregnancy and childbirth.
- Pregnant women infected with Ebola virus may experience miscarriage, stillbirth, or maternal death, highlighting the importance of pregnancy surveillance and obstetric care in Ebola-affected areas.
Managing the complications of Ebola virus disease requires comprehensive supportive care, including fluid resuscitation, electrolyte replacement, organ support, and treatment of secondary infections.
How is Ebola virus disease prevented?
Preventing Ebola virus disease (EVD) requires a multi-faceted approach that encompasses public health measures, community engagement, and individual behavior change. Given the severity and potential for outbreaks, prevention strategies focus on reducing the risk of Ebola virus transmission and controlling its spread. Here are key components of Ebola virus disease prevention:
Surveillance and early detection:
- Early detection of Ebola cases is critical for implementing timely interventions and preventing outbreaks. Surveillance systems monitor for suspected cases, identify contacts of infected individuals, and track disease transmission within communities.
- Rapid diagnostic tests and laboratory confirmation of Ebola virus infection enable prompt isolation of cases and implementation of infection control measures.
Infection control measures:
- Strict infection control practices are essential for preventing Ebola virus transmission in healthcare settings and communities.
- Healthcare workers must adhere to standard precautions, including hand hygiene, wearing personal protective equipment (PPE) such as gloves, gowns, masks, and eye protection, and implementing safe waste management practices.
- Isolation of suspected and confirmed cases, along with appropriate environmental disinfection, helps minimize the risk of transmission to healthcare workers and other patients.
Safe burial practices:
- Traditional burial practices, such as washing and touching the body of the deceased, can contribute to Ebola virus transmission. Promoting safe burial practices that minimize contact with the deceased, such as cremation or burial in sealed body bags, helps prevent further spread of the virus.
Community engagement and education:
- Engaging communities in Ebola prevention efforts is essential for building trust, addressing misconceptions, and promoting behavior change.
- Community health workers play a crucial role in disseminating accurate information about Ebola virus transmission, symptoms, and preventive measures.
- Educational campaigns emphasize the importance of hand hygiene, avoiding contact with sick individuals or bodily fluids, and seeking medical care promptly if symptoms develop.
Border health and travel restrictions:
- Monitoring and screening travelers at international borders and points of entry help identify individuals at risk of Ebola virus exposure and prevent importation of cases.
- Travel restrictions and quarantine measures may be implemented during Ebola outbreaks to limit the spread of the virus across borders and regions.
Vaccination:
- Vaccination can play a key role in preventing Ebola virus disease outbreaks. The rVSV-ZEBOV vaccine has shown efficacy in clinical trials and is used for Ebola outbreak response and pre-exposure vaccination of healthcare workers and at-risk populations.
- Vaccination campaigns target frontline healthcare workers, contacts of confirmed cases, and individuals at high risk of exposure in outbreak-affected areas.
Research and development:
- Continued investment in research and development is essential for advancing Ebola prevention and control strategies.
- Ongoing research focuses on developing new vaccines, antiviral drugs, and diagnostic tests, as well as understanding the ecology of Ebola virus transmission and improving outbreak preparedness and response capabilities.
Takeaway
Ebola virus disease is a severe and often fatal illness caused by infection with the Ebola virus. It is characterized by symptoms such as fever, severe headache, muscle pain, weakness, fatigue, diarrhea, vomiting, abdominal pain, and unexplained bleeding or bruising. Early detection and prompt medical intervention are crucial for improving outcomes and reducing the morbidity and mortality associated with EVD. Preventing Ebola virus disease requires a collaborative and sustained effort involving governments, healthcare organizations, community leaders, international partners, and individuals.
Frequently Asked Questions
Q: What is Ebola virus disease (EVD)?
A: Ebola virus disease (EVD) is a severe and often fatal illness caused by infection with the Ebola virus. It can affect humans and other primates, leading to symptoms such as fever, headache, muscle pain, weakness, vomiting, diarrhea, and in some cases, unexplained bleeding.
Q: How is Ebola virus transmitted?
A: Ebola virus is primarily transmitted through direct contact with the bodily fluids of infected individuals or animals. This includes blood, saliva, vomit, urine, feces, sweat, semen, and other bodily fluids. Transmission can occur through broken skin or mucous membranes, as well as indirect contact with contaminated surfaces or objects.
Q: What are the symptoms of Ebola virus disease?
A: Symptoms of Ebola virus disease typically include fever, headache, muscle pain, weakness, vomiting, diarrhea, abdominal pain, and unexplained bleeding or bruising. These symptoms can vary in severity and may progress rapidly, leading to severe dehydration, organ failure, and death in some cases.
Q: How is Ebola virus disease diagnosed?
A: Diagnosis of Ebola virus disease involves clinical assessment, laboratory testing, and epidemiological investigation. Healthcare providers evaluate patients for symptoms consistent with EVD, obtain medical history and travel history, and collect blood samples for laboratory testing to confirm the presence of Ebola virus genetic material (RNA).
Q: What is the treatment for Ebola virus disease?
A: There is no specific antiviral treatment for Ebola virus disease. Treatment primarily focuses on supportive care to manage symptoms, prevent complications, and improve the patient’s chances of survival. This includes fluid and electrolyte replacement, management of fever and pain, nutritional support, and treatment of complications such as organ failure and secondary infections.
Q: How can Ebola virus disease be prevented?
A: Prevention of Ebola virus disease involves a combination of public health measures, community engagement, and individual behavior change. Strategies include surveillance and early detection of cases, infection control measures in healthcare settings, promoting safe burial practices, community education, vaccination, and research and development of new preventive measures.
References
- World Health Organization. (2020). Ebola virus disease. https://www.who.int/health-topics/ebola/#tab=tab_1
- Centers for Disease Control and Prevention. (2021). Ebola (Ebola virus disease). https://www.cdc.gov/vhf/ebola/index.html
- Feldmann, H., & Geisbert, T. W. (2011). Ebola haemorrhagic fever. The Lancet, 377(9768), 849-862. https://doi.org/10.1016/S0140-6736(10)60667-8
- Muyembe-Tamfum, J. J., Mulangu, S., Masumu, J., & Kayembe, J. M. (2012). Ebola virus outbreaks in Africa: past and present. Onderstepoort Journal of Veterinary Research, 79(2), 451. https://doi.org/10.4102/ojvr.v79i2.451
- World Health Organization. (2020). Ebola virus disease: fact sheet. https://www.who.int/news-room/fact-sheets/detail/ebola-virus-disease
- Geisbert, T. W., & Jahrling, P. B. (2004). Exotic emerging viral diseases: progress and challenges. Nature Medicine, 10(12s), S110-S121. https://doi.org/10.1038/nm1142