Types | Transmission | Symptoms | Diagnosis | Treatment | Complications | Prevention | Takeaway | FAQs
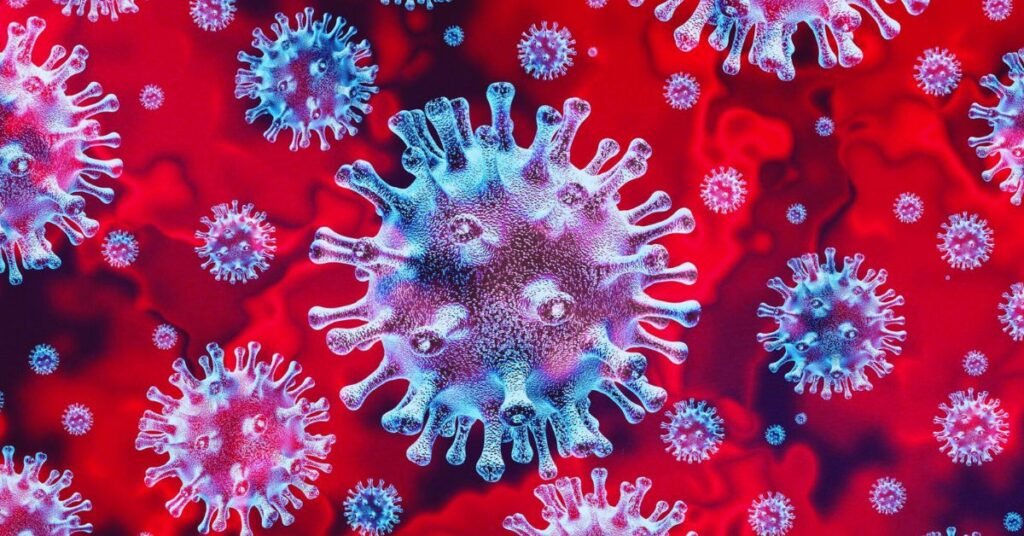
Coronaviruses are a family of viruses that can infect both humans and animals. They are named for the crown-like spikes that protrude from their surfaces when viewed under a microscope.
What is coronavirus disease?
Coronavirus Disease, commonly known as COVID-19, is a highly contagious respiratory illness caused by a novel coronavirus called SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2). The disease was first identified in Wuhan, China, in December 2019 and has since evolved into a global pandemic, impacting nearly every corner of the world.
What are the types of coronaviruses?
There are several types of coronaviruses, with some of the most notable ones being:
Common human coronaviruses:
- HCoV-229E: This virus can cause mild to moderate upper respiratory tract infections, such as the common cold.
- HCoV-NL63: Like HCoV-229E, this virus primarily causes mild respiratory symptoms in humans.
- HCoV-OC43: It is associated with common cold symptoms but can also lead to more severe lower respiratory tract infections, especially in the elderly and individuals with weakened immune systems.
- HCoV-HKU1: This virus can cause respiratory infections and is sometimes linked to severe respiratory diseases in vulnerable populations.
Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV):
- SARS-CoV caused the Severe Acute Respiratory Syndrome (SARS) outbreak in 2002-2003, primarily in Asia. It had a high mortality rate and resulted in significant global public health concerns. The disease is characterized by severe respiratory symptoms, including fever, cough, and difficulty breathing.
Middle East Respiratory Syndrome Coronavirus (MERS-CoV):
- MERS-CoV was responsible for the Middle East Respiratory Syndrome (MERS) outbreak, first identified in Saudi Arabia in 2012. MERS is a severe respiratory illness with a relatively high mortality rate. It can lead to pneumonia and acute respiratory distress.
Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2):
- SARS-CoV-2 is responsible for the Coronavirus Disease 2019 (COVID-19) pandemic that began in late 2019. COVID-19 presents a wide range of symptoms, from mild or asymptomatic cases to severe respiratory illness, multi-organ failure, and death. This ongoing pandemic has resulted in significant global health, economic, and social impacts.
Animal coronaviruses:
- Several coronaviruses primarily affect animals, including domestic animals like dogs, cats, and livestock. One notable example is Canine Coronavirus (CCoV) in dogs, which causes gastrointestinal symptoms. Feline Coronavirus (FCoV) affects cats, causing mild enteric symptoms. Additionally, several animal coronaviruses can undergo genetic mutations and cross into humans, as seen with the origins of SARS, MERS, and COVID-19.
New variants:
- As the SARS-CoV-2 virus continues to circulate and infect individuals, it has undergone genetic changes, leading to the emergence of new variants. Some of these variants have exhibited increased transmissibility, altered disease severity, or potential resistance to immunity from previous infections or vaccines. Continuous surveillance and research are ongoing to monitor these variants and adapt public health strategies accordingly.
How is coronavirus disease transmitted?
SARS-CoV-2 is thought to have its origins in bats and potentially transitioned to humans via an intermediary animal host. It is thought that the virus may have first emerged in a seafood market in Wuhan, China, where live animals were also sold. This zoonotic transmission is not uncommon with coronaviruses, as previous outbreaks, like Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS), also had their origins in animals before infecting humans. Here’s how COVID-19 is transmitted:
Respiratory droplets: The most common mode of transmission for COVID-19 is through respiratory droplets produced when an infected person talks, coughs, sneezes, or even breathes. These droplets contain viral particles, and if a person inhales these droplets, they can become infected.
Close contact: COVID-19 transmission is most likely to occur in close contact with an infected person. Close contact is typically defined as being within 6 feet (about 2 meters) of an infected individual for an extended period, especially in indoor settings with poor ventilation.
Airborne transmission: While respiratory droplets are the primary mode of transmission, there is also evidence to suggest that in certain conditions, the virus can become aerosolized, meaning it can linger in the air for an extended period. This is more likely in enclosed spaces with poor ventilation, and it underscores the importance of mask-wearing and improved ventilation measures in such environments.
Fomite transmission: Another potential mode of transmission is through contact with contaminated surfaces and objects, known as fomite transmission. If an infected person touches their face and then touches surfaces like doorknobs, countertops, or personal items, the virus can be left behind. If someone else touches these contaminated surfaces and then touches their face, they can become infected. Proper hand hygiene is essential to reduce fomite transmission.
Pre-symptomatic and asymptomatic transmission: Individuals infected with COVID-19 can spread the virus to others even before they show symptoms (pre-symptomatic transmission) or when they never develop noticeable symptoms (asymptomatic transmission). This complicates efforts to control the spread of the virus, as carriers who feel well can unknowingly transmit the virus to others.
Close contact and crowded settings: Close contact in crowded, enclosed spaces, such as public transportation, offices, restaurants, and households, increases the risk of transmission. Physical distancing and reduced occupancy measures are used to mitigate this risk.
Super-spreader events: COVID-19 transmission can be amplified by super-spreader events, where one infected person can infect a large number of individuals. These events often occur at gatherings or in settings with conditions that facilitate close contact and the release of respiratory droplets.
What are the symptoms of coronavirus disease?
Coronavirus Disease (COVID-19) can manifest with a wide range of symptoms, from mild to severe, and in some cases, it can be asymptomatic (showing no symptoms).

Common symptoms:
- Fever: Elevated body temperature, often one of the first signs of COVID-19.
- Cough: A dry or productive cough is a prevelant symptom.
- Shortness of breath: Difficulty in breathing or breathlessness, particularly in severe cases.
- Fatigue: Feeling unusually tired or lethargic.
- Muscle aches and body pains: Generalized body aches and muscle soreness.
- Headache: Frequently reported in COVID-19 cases.
- Sore Throat: A scratchy or painful throat, sometimes accompanied by difficulty swallowing.
- Loss of taste or smell (Anosmia): A sudden and unexplained loss of the ability to taste or smell.
- Congestion and runny nose: Symptoms that can resemble a common cold.
- Gastrointestinal symptoms: These may encompass feelings of nausea, episodes of vomiting, instances of diarrhea, or discomfort in the abdominal region.
Less common and severe symptoms:
- Respiratory symptoms: COVID-19 can lead to severe respiratory distress, with symptoms such as severe shortness of breath, chest pain, and a persistent cough.
- High blood pressure: Some individuals with COVID-19 experience elevated blood pressure.
- Confusion or altered mental state: This is more common in severe cases and may be a sign of neurological involvement.
- Skin rashes: Some COVID-19 patients develop skin rashes or hives.
- COVID toes: This peculiar symptom involves the development of painful, discolored toes or fingers.
- Persistent chest pain: This may be a sign of severe lung involvement and should be evaluated promptly.
- Blood clots: COVID-19 is associated with an increased risk of blood clots, which can lead to more severe complications like stroke or pulmonary embolism.
- Multisystem inflammatory syndrome in children (MIS-C): This rare but severe condition primarily affects children and can cause persistent fever, inflammation, and multiple organ involvement.
It’s crucial to emphasize that COVID-19 symptoms can differ from one individual to another. Additionally, severe cases can potentially lead to hospitalization, respiratory failure, or death, especially in vulnerable populations such as the elderly and those with underlying health conditions.
How is coronavirus disease diagnosed?

The diagnosis of Coronavirus Disease (COVID-19) is typically made through a combination of clinical evaluation, symptoms assessment, and laboratory testing. Here’s a detailed explanation of how COVID-19 is diagnosed:
Clinical evaluation
Healthcare providers assess a person’s medical history, travel history, and exposure to confirmed COVID-19 cases.
Symptoms are discussed and evaluated, as COVID-19 can present with a wide range of symptoms, from mild to severe.
The clinical evaluation may include physical examinations, focusing on respiratory symptoms and vital signs.
Laboratory testing
Polymerase chain reaction (PCR) test: This is the most common and accurate diagnostic test for COVID-19. It detects the presence of the virus’s genetic material (RNA) in respiratory specimens, typically collected via a nasal or throat swab. Results are usually available within a few hours to a few days, depending on testing capacity and local resources.
Rapid Antigen test: This test is similar to PCR but provides quicker results (usually within 15-30 minutes). It detects specific viral proteins in respiratory samples. While less sensitive than PCR, rapid tests are valuable for mass screening and quick confirmation of cases.
Serology or antibody test: These blood tests identify the presence of antibodies against the virus. They can indicate a past infection but are less effective for diagnosing active cases. Antibodies may take several days to weeks to develop after infection.
Serum neutralization assay: This specialized test measures a person’s ability to neutralize the virus. It’s often used in research and vaccine development.
Imaging
Chest X-rays and computed tomography (CT) scans are sometimes used to assess lung involvement, especially in cases with severe respiratory symptoms. Ground-glass opacities and other characteristic patterns on imaging may suggest COVID-19.
Point-of-care testing:
Some locations, such as healthcare facilities, airports, and testing centers, offer point-of-care testing with rapid results. These tests are helpful for quickly identifying and isolating positive cases.
Contact tracing:
Identifying and notifying individuals who have been in close contact with a confirmed case is a crucial part of the diagnosis and control process. Contact tracing helps contain the spread of the virus by isolating and testing potentially exposed individuals.
Home test kits:
Over-the-counter at-home COVID-19 test kits are available in some regions. These tests often use nasal swabs and provide results at home. They are a useful tool for self-monitoring and early detection.
Saliva tests:
Saliva tests have gained popularity as a less invasive method for sample collection. They work on similar principles as PCR tests, detecting viral RNA in saliva.
It’s important to note that the accuracy of test results can vary based on factors like the timing of the test, the quality of the sample collected, and the type of test used. False-negative and false-positive results can occur, so clinical judgment is essential when interpreting test outcomes.
What is the treatment for coronavirus disease?
The treatment for Coronavirus Disease (COVID-19) primarily involves supportive care, as there is no specific antiviral medication approved to treat the SARS-CoV-2 virus directly.

- Supportive care: Most COVID-19 cases are mild and can be managed at home with rest, hydration, and over-the-counter medications to alleviate symptoms. These medications can include fever reducers (e.g., acetaminophen) and cough suppressants.
- Hospitalization: Admission to the hospital may be necessary for severe cases or individuals with preexisting health conditions. Hospital care is focused on monitoring and treating severe respiratory symptoms, as well as addressing potential complications.
- Oxygen therapy: In cases of hypoxia (low blood oxygen levels), supplemental oxygen is provided through devices such as nasal cannulas, face masks, or ventilators. High-flow nasal cannula therapy and non-invasive positive pressure ventilation (NIPPV) are also used to improve oxygenation.
- Steroids: In some severe cases with significant inflammation and lung involvement, corticosteroids like dexamethasone may be used to reduce inflammation and improve respiratory function.
- Antiviral medications: Some antiviral medications, such as remdesivir, have been authorized for emergency use in hospitalized COVID-19 patients. However, their effectiveness varies and they are not a cure.
- Monoclonal antibody therapy: Monoclonal antibody treatments, like bamlanivimab and etesevimab, have been developed and authorized for use in certain cases, primarily in high-risk individuals with mild to moderate COVID-19. These therapies aim to reduce the severity of symptoms and the risk of progression to severe disease.
- Convalescent plasma: Convalescent plasma therapy involves using blood plasma from individuals who have recovered from COVID-19 and have developed antibodies against the virus. This treatment is used to boost the immune response in some cases.
- Vaccination: Prevention is a crucial aspect of managing COVID-19. Vaccination has been a key tool in reducing the spread of the virus, preventing severe illness, and saving lives. Widespread vaccination efforts are essential in controlling the pandemic.
- Pulmonary rehabilitation: For individuals who experience severe respiratory complications, such as acute respiratory distress syndrome (ARDS), post-recovery pulmonary rehabilitation may be necessary to help restore lung function and physical well-being.
- Mental health support: COVID-19 can have mental health effects, including anxiety, depression, and post-traumatic stress. Psychological support and counseling services are important components of comprehensive care.
It’s crucial to note that the management of COVID-19 varies based on the severity of the illness and the individual’s overall health.
What are the complications of coronavirus disease?
Coronavirus Disease (COVID-19) can lead to a variety of complications, ranging from mild to severe, with some having long-lasting effects.
Respiratory complications:
- Pneumonia: COVID-19 can cause severe lung inflammation, leading to pneumonia, which can be life-threatening.
- Acute Respiratory Distress Syndrome (ARDS): Severe cases may progress to ARDS, a condition where the lungs fill with fluid, causing severe oxygen deficiency.
- Chronic respiratory issues: Some COVID-19 survivors experience lingering respiratory problems, including shortness of breath, cough, and reduced lung function.
Cardiovascular complications:
- Heart damage: COVID-19 has been associated with heart inflammation (myocarditis) and damage to the heart muscle, which can lead to heart failure and other cardiac issues.
- Blood clots: The virus can increase the risk of blood clots, which can lead to conditions like deep vein thrombosis (DVT), pulmonary embolism, or stroke.
Neurological complications:
- Loss of smell and taste: Anosmia and ageusia, or loss of smell and taste, are common neurological symptoms of COVID-19.
- Neurological symptoms: Some individuals may experience confusion, dizziness, headaches, and neurological symptoms that require further evaluation.
- Guillain-Barré Syndrome: In rare cases, COVID-19 has been associated with Guillain-Barré syndrome, a disorder affecting the nerves.
Kidney and liver complications:
- Kidney injury: COVID-19 can lead to acute kidney injury, particularly in severe cases.
- Liver dysfunction: Some patients may develop liver inflammation, which can cause liver function abnormalities.
Gastrointestinal complications:
- Gastrointestinal symptoms: Nausea, vomiting, diarrhea, and abdominal pain can be part of the symptom profile.
- GI bleeding: Severe cases may result in gastrointestinal bleeding.
Multi-organ dysfunction:
COVID-19 can affect multiple organs, leading to multi-organ failure in severe cases.
Post-Acute Sequelae of SARS-CoV-2 Infection (PASC):
Some individuals, often referred to as “long-haulers,” experience prolonged symptoms and complications, including fatigue, shortness of breath, chest pain, joint pain, and cognitive issues, for several weeks or months after recovery from the acute phase of the disease.
Secondary infections:
Pneumonia or other bacterial infections can occur as secondary complications during the course of COVID-19.
Psychological and mental health effects:
The pandemic has been associated with a rise in mental health issues, including anxiety, depression, post-traumatic stress disorder (PTSD), and other stress-related conditions.
Impact on pre-existing conditions:
COVID-19 can exacerbate existing health conditions, such as diabetes, hypertension, and respiratory diseases, leading to complications and challenges in disease management.
It’s important to note that the severity and likelihood of these complications can vary depending on an individual’s age, overall health, and the course of the disease.
How is coronavirus disease be prevented?
Preventing Coronavirus Disease (COVID-19) involves a combination of individual and community-level measures to reduce the transmission of the virus.
Vaccination: Getting vaccinated is one of the most effective ways to prevent COVID-19 and its severe consequences. Vaccines have been approved for emergency use in many countries. Widespread vaccination helps achieve herd immunity and reduces the spread of the virus.

Face masks: Wearing masks, particularly in indoor and crowded settings, helps reduce the transmission of respiratory droplets that may contain the virus. Masks are particularly effective when both the infected and uninfected individuals wear them.
Physical distancing: Maintaining a safe distance (at least 6 feet or 2 meters) from individuals outside your household can reduce the risk of respiratory droplet transmission.
Hand hygiene: Regularly washing hands with soap and water for at least 20 seconds or using hand sanitizers with at least 60% alcohol is crucial in reducing the risk of contact transmission from contaminated surfaces.
Avoiding touching the face: Avoiding touching the eyes, nose, and mouth with unwashed hands can reduce the risk of introducing the virus into the body.
Respiratory hygiene: Covering your mouth and nose with a tissue or your elbow when coughing or sneezing can prevent the release of respiratory droplets containing the virus.
Good ventilation: Ensuring adequate ventilation in indoor spaces by opening windows and using air purifiers can reduce the concentration of viral particles in the air.
Quarantine and isolation: Individuals who have been exposed to COVID-19 or are confirmed to have the virus should follow quarantine and isolation guidelines. This prevents further transmission. Quarantine is for those exposed but not yet infected, while isolation is for those who are infected.
Testing: Regular testing and timely isolation of individuals with COVID-19 can help break the chain of transmission.
Travel restrictions and guidelines: Following travel guidelines, including testing requirements and quarantine measures, can help prevent the spread of the virus across regions.
Avoiding crowded and close-contact settings: Reducing participation in crowded events and avoiding close-contact situations with individuals outside your household can mitigate the risk of exposure.
Community engagement and education: Promoting public awareness through community engagement, education, and outreach efforts helps ensure that individuals are well-informed about COVID-19 and the measures they can take to prevent it.
Takeaway
Coronavirus Disease has altered our lives in profound ways, and staying informed is our best defense. While efforts are ongoing to develop more effective treatments, prevention through vaccination and public health measures, such as mask-wearing, physical distancing, and hand hygiene, remains the most effective way to reduce the spread of the virus and the impact of the disease. Individuals with COVID-19 symptoms or confirmed cases should follow healthcare provider recommendations and isolation protocols to prevent further transmission.
Frequently Asked Questions
Q: Is there a cure for COVID-19?
A: There is no specific antiviral cure for COVID-19. Treatment mainly involves supportive care and, in severe cases, may include oxygen therapy, steroids, and other medications to manage symptoms.
Q: How can I protect myself from COVID-19?
A: You can protect yourself by getting vaccinated, wearing masks, practicing good hand hygiene, maintaining physical distance, and avoiding crowded and close-contact settings.
Q: What is herd immunity, and how is it achieved?
A: Herd immunity occurs when a sufficient portion of the population is immune to the virus, either through vaccination or previous infection, reducing the spread of the virus within the community.
Q: Are COVID-19 vaccines safe and effective?
A: Yes, COVID-19 vaccines have undergone rigorous testing to ensure safety and efficacy. They are highly effective in reducing the severity of illness and the spread of the virus.
Q: Can I get COVID-19 even if I’m fully vaccinated?
A: While vaccination greatly reduces the risk of severe illness, it is still possible to get infected. These cases are often milder, and the vaccine remains a crucial tool in preventing the spread of the virus.
Q: What are the long-term effects of COVID-19?
A: Some individuals experience long-term symptoms, referred to as “long COVID,” including fatigue, shortness of breath, cognitive issues, and other lingering health problems.
Q: Are there variants of the virus, and do they impact the effectiveness of vaccines?
A: Yes, there are variants of SARS-CoV-2. Some may affect vaccine effectiveness, but vaccines continue to provide protection against severe illness.
Q: What should I do if I’ve been in close contact with a confirmed case of COVID-19?
A: Follow quarantine guidelines, get tested, and monitor for symptoms. Isolation may be necessary if you become infected.
Q: Is it safe to travel during the pandemic?
A: Traveling is associated with some risk. Follow travel guidelines, get vaccinated, and take precautions to minimize exposure and transmission.
References
- Centers for Disease Control and Prevention (CDC). (2020). COVID-19 (Coronavirus Disease 2019). Link
- Johns Hopkins University. (2020). COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE). Link
- National Institutes of Health (NIH). (2020). Coronavirus Disease 2019 (COVID-19). Link
- Nature. (2020). Coronavirus latest. Link
- The Lancet. (2020). COVID-19 Resource Centre. Link
- New England Journal of Medicine. (2020). Coronavirus (Covid-19). Link