Causes | Symptoms | Diagnosis | Treatment | Complications | Prevention | Takeaway | FAQs
Rheumatoid arthritis (RA) is a type of arthritis where the immune system mistakenly attacks the body’s own tissues, particularly the synovium – the lining of the membranes that surround the joints. It is different from osteoarthritis, which is caused by wear and tear on the joints.
What is rheumatoid arthritis?
Rheumatoid arthritis (RA) is a chronic autoimmune disorder characterized by inflammation of the joints, which leads to pain, swelling, stiffness, and eventually joint damage and deformity. It can also affect other parts of the body, such as the skin, eyes, lungs, and blood vessels.
What causes rheumatoid arthritis?
While the exact cause of rheumatoid arthritis is not fully understood, researchers believe that it involves a combination of genetic, environmental, and hormonal factors.
- Genetic factors: Genetics play a significant role in the development of rheumatoid arthritis. Individuals with a family history of RA are at a higher risk of developing the condition. Certain genetic markers, such as specific variations in genes related to the immune system, have been associated with an increased susceptibility to RA. However, having these genetic predispositions does not guarantee the development of the disease, indicating that other factors are also involved.
- Autoimmune response: Rheumatoid arthritis is considered an autoimmune disease, meaning that the body’s immune system mistakenly attacks its own tissues. In RA, the immune system targets the synovium, the lining of the membranes that surround the joints. This leads to chronic inflammation, which can result in joint damage and deformities over time. The exact trigger for this autoimmune response is not fully understood, but it is believed to involve a combination of genetic susceptibility and environmental factors.
- Environmental factors: Environmental factors may also contribute to the development of rheumatoid arthritis. These factors include exposure to certain infections, such as viruses and bacteria, which may trigger an abnormal immune response in susceptible individuals. Additionally, exposure to environmental toxins, such as cigarette smoke, may increase the risk of developing RA or exacerbate symptoms in individuals who already have the condition.
- Hormonal factors: Hormonal factors, particularly the role of estrogen, have been implicated in the development of rheumatoid arthritis. Women are more likely to develop RA than men, and the onset of the disease often coincides with hormonal changes, such as puberty, pregnancy, and menopause. Estrogen has been shown to have immunomodulatory effects, and fluctuations in estrogen levels may influence the activity of the immune system and contribute to the development or progression of RA in susceptible individuals.
- Other factors: Several other factors may also contribute to the development of rheumatoid arthritis or exacerbate symptoms in individuals who already have the condition. These include obesity, which increases mechanical stress on the joints and promotes inflammation, as well as certain lifestyle factors such as diet and stress, which may influence immune function and inflammation levels.
What are the symptoms of rheumatoid arthritis?
The symptoms of RA can vary from person to person and may fluctuate in intensity over time. Here are the common symptoms associated with rheumatoid arthritis:

- Joint pain: Persistent joint pain, often described as a dull ache or throbbing sensation, is a hallmark symptom of RA. The pain may be present in multiple joints simultaneously and is typically worse in the morning or after periods of inactivity.
- Joint stiffness: Stiffness in the affected joints, especially in the morning or after prolonged periods of rest, is a common symptom of rheumatoid arthritis. This stiffness can make it difficult to move the joints, and it usually improves with movement and activity throughout the day.
- Joint swelling: Inflammation of the synovium (the lining of the joint capsule) leads to swelling and tenderness in the affected joints. Swollen joints may appear red and feel warm to the touch.
- Joint warmth: Increased blood flow to inflamed joints can cause them to feel warm to the touch. This warmth may be noticeable even without visible swelling.
- Joint redness: Inflamed joints may appear red and shiny due to increased blood flow and swelling of the synovial tissue.
- Joint fatigue: Joint fatigue or weakness can occur as a result of ongoing inflammation and damage to the joints. This may manifest as a feeling of heaviness or weakness in the affected joints.
- Morning stiffness: Many individuals with RA experience prolonged morning stiffness lasting for at least 30 minutes or more. This stiffness may improve with movement but can be a significant challenge upon waking.
- Symmetrical joint involvement: Rheumatoid arthritis typically affects joints on both sides of the body symmetrically. For example, if the knuckles of one hand are affected, the corresponding knuckles on the other hand are likely to be affected as well.
- Fatigue: Chronic inflammation and the stress of living with a chronic condition can lead to persistent fatigue in individuals with RA. This fatigue may be more severe during disease flares or after engaging in physical activity.
- Systemic symptoms: In addition to joint-related symptoms, rheumatoid arthritis can also cause systemic symptoms such as fever, loss of appetite, weight loss, and generalized malaise. These symptoms may occur during disease flares or as a result of complications related to RA.
- Nodules: Some individuals with rheumatoid arthritis may develop firm, round nodules under the skin, typically near the affected joints. These nodules, known as rheumatoid nodules, are often painless but can become inflamed and tender in some cases.
- Joint deformities: Over time, untreated rheumatoid arthritis can lead to joint deformities and functional impairment. Joint deformities may include misalignment, subluxation (partial dislocation), or even complete destruction of the joint structure.
It’s important to note that the severity and combination of symptoms can vary widely among individuals with rheumatoid arthritis.
How is rheumatoid arthritis diagnosed?
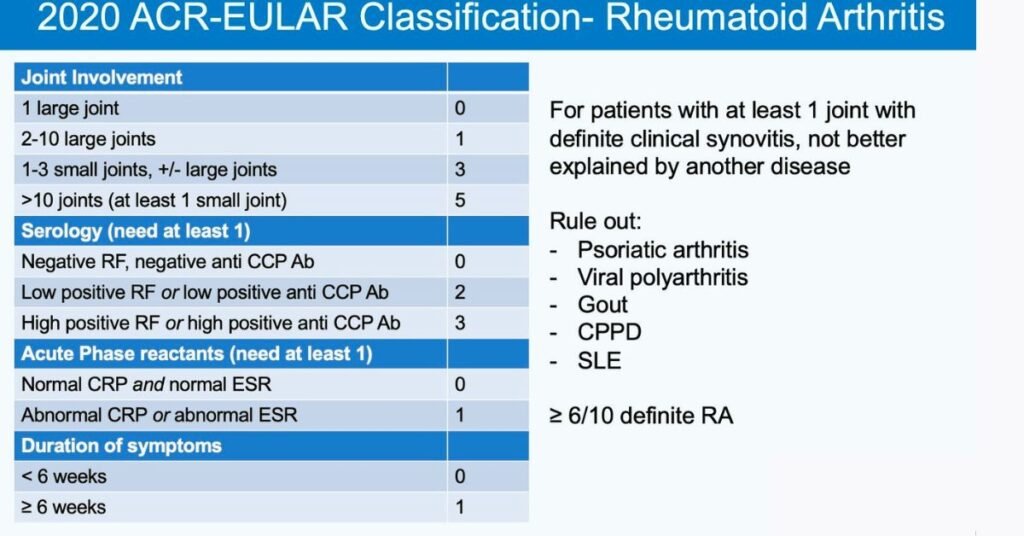
Diagnosing rheumatoid arthritis involves a combination of medical history, physical examination, laboratory tests, and imaging studies. Since RA shares symptoms with other types of arthritis and autoimmune diseases, a comprehensive approach is necessary for an accurate diagnosis.
Medical history: The healthcare provider will begin by taking a detailed medical history, including symptoms, their onset, duration, and any factors that worsen or alleviate them. They will also inquire about family history of autoimmune diseases, previous joint injuries or infections, and any other relevant medical conditions.
Physical examination: A thorough physical examination will be conducted to assess joint function, swelling, tenderness, warmth, and range of motion. The healthcare provider will examine multiple joints throughout the body, as rheumatoid arthritis can affect joints symmetrically. They may also look for signs of inflammation, such as redness and swelling.
Laboratory tests: Blood tests are commonly used to aid in the diagnosis of rheumatoid arthritis and assess disease activity. These tests may include:
- Rheumatoid factor (RF): RF is an antibody present in the blood of many individuals with rheumatoid arthritis. However, it can also be found in other autoimmune diseases and some healthy individuals.
- Anti-cyclic citrullinated peptide (anti-CCP) antibodies: These antibodies are more specific to rheumatoid arthritis and are often present in individuals with the disease, especially in early stages.
- C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR): These markers of inflammation are often elevated in individuals with active rheumatoid arthritis, although they are not specific to RA and can be elevated in other conditions as well.
- Complete blood count (CBC): A CBC may reveal anemia, which is common in individuals with RA due to chronic inflammation.
Imaging studies: Imaging studies such as X-rays, ultrasound, or magnetic resonance imaging (MRI) may be performed to assess joint damage and inflammation. These imaging modalities can help detect joint erosions, soft tissue swelling, and synovial inflammation characteristic of rheumatoid arthritis. X-rays may also be used to monitor disease progression over time.
Other tests: In some cases, additional tests may be performed to rule out other conditions that can mimic rheumatoid arthritis or to evaluate for complications of the disease. These may include joint aspiration (removing fluid from a swollen joint for analysis), bone scans, or tests for infectious agents.
Diagnostic criteria: The American College of Rheumatology (ACR) and the European League Against Rheumatism (EULAR) have established classification criteria for rheumatoid arthritis based on clinical and laboratory parameters. Meeting these criteria can aid in the diagnosis of RA and guide treatment decisions.
How is rheumatoid arthritis treated?
Treatment for rheumatoid arthritis aims to alleviate symptoms, reduce inflammation, slow disease progression, preserve joint function, and improve overall quality of life.
Medications:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs such as ibuprofen, naproxen, and aspirin can help relieve pain and reduce inflammation in individuals with RA. They are often used to manage mild to moderate symptoms.
- Disease-modifying antirheumatic drugs (DMARDs): DMARDs are the cornerstone of RA treatment and work to slow or halt the progression of the disease by suppressing the immune system. Methotrexate is the most commonly prescribed DMARD for RA, but other options include hydroxychloroquine, sulfasalazine, leflunomide, and azathioprine.
- Biologic DMARDs: Biologic DMARDs, also known as biologics, target specific components of the immune system involved in the inflammatory process. These drugs are typically reserved for individuals with moderate to severe RA who have not responded adequately to conventional DMARDs. Examples include TNF-alpha inhibitors (e.g., etanercept, adalimumab), interleukin-6 (IL-6) inhibitors (e.g., tocilizumab), and B-cell inhibitors (e.g., rituximab).
- Janus kinase (JAK) inhibitors: JAK inhibitors are a newer class of DMARDs that work by blocking the action of enzymes involved in the inflammatory response. Tofacitinib and baricitinib are examples of JAK inhibitors approved for the treatment of RA.
- Corticosteroids: Corticosteroids, such as prednisone, may be used to rapidly reduce inflammation and alleviate symptoms during RA flares. However, long-term use of corticosteroids is generally avoided due to the risk of side effects, including osteoporosis, weight gain, and increased susceptibility to infections.
Lifestyle modifications:
- Exercise: Regular exercise, including aerobic exercise, strength training, and flexibility exercises, can help improve joint function, reduce pain, and maintain mobility in individuals with RA. Low-impact activities such as swimming, walking, and cycling are often recommended.
- Healthy diet: A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and omega-3 fatty acids may help reduce inflammation and support overall health in individuals with RA. Some research suggests that certain dietary supplements, such as fish oil and turmeric, may have anti-inflammatory effects.
- Stress management: Stress can exacerbate RA symptoms, so techniques such as relaxation exercises, meditation, and mindfulness may help reduce stress levels and improve coping abilities.
Physical therapy:
- Physical therapy can help individuals with RA improve joint function, strength, and flexibility through targeted exercises and techniques. A physical therapist can also provide guidance on joint protection strategies and assistive devices to help minimize pain and disability.
Surgery:
- In severe cases of RA where joint damage is extensive and debilitating, surgery may be necessary to repair or replace damaged joints. Common surgical procedures for RA include joint replacement surgery (e.g., hip or knee replacement) and joint fusion (arthrodesis) to stabilize and immobilize severely damaged joints.
Complementary and alternative therapies:
- Some individuals with RA may find relief from complementary and alternative therapies such as acupuncture, massage therapy, chiropractic care, and herbal supplements. While these therapies may help manage symptoms for some individuals, it’s essential to discuss their use with a healthcare provider to ensure they are safe and effective.
Overall, the treatment of rheumatoid arthritis is individualized based on the severity of symptoms, disease activity, comorbidities, and patient preferences. Early diagnosis and aggressive treatment are essential for controlling inflammation, preventing joint damage, and optimizing long-term outcomes for individuals with RA.
What are the complications of rheumatoid arthritis?
While joint inflammation and damage are the hallmark features of RA, the disease can lead to various complications affecting different parts of the body.
- Joint damage and deformities: Persistent inflammation in the joints can lead to progressive damage and erosion of the cartilage and bone, resulting in joint deformities, instability, and functional impairment. Common joint deformities seen in RA include:
- Swan-neck deformity: Characterized by hyperextension of the proximal interphalangeal joint and flexion of the distal interphalangeal joint in the fingers.
- Boutonniere deformity: Involves flexion of the proximal interphalangeal joint and hyperextension of the distal interphalangeal joint in the fingers.
- Ulnar deviation: Deviation of the fingers towards the ulnar side of the hand due to tendon imbalance and joint destruction.
- Joint destruction and disability: Severe and prolonged inflammation can lead to irreversible joint damage, loss of joint function, and disability in individuals with RA. Joint destruction may necessitate surgical interventions such as joint replacement surgery (arthroplasty) or joint fusion (arthrodesis) to restore stability and function.
- Cardiovascular complications: Rheumatoid arthritis is associated with an increased risk of cardiovascular disease, including heart attacks, strokes, and peripheral arterial disease. Chronic inflammation in RA can lead to accelerated atherosclerosis (hardening and narrowing of the arteries), endothelial dysfunction, and increased risk of blood clots.
- Rheumatoid nodules: Rheumatoid nodules are firm, rounded masses that develop under the skin, typically over bony prominences or areas of repeated pressure. These nodules are composed of inflammatory tissue and can range in size from small pea-sized bumps to larger masses. While rheumatoid nodules are usually painless, they can become inflamed, tender, or ulcerated in some cases.
- Osteoporosis and bone loss: Chronic inflammation and the use of corticosteroids to manage RA symptoms can increase the risk of osteoporosis (reduced bone density) and fractures in individuals with RA. Osteoporosis may further exacerbate joint damage and increase the risk of disability in affected individuals.
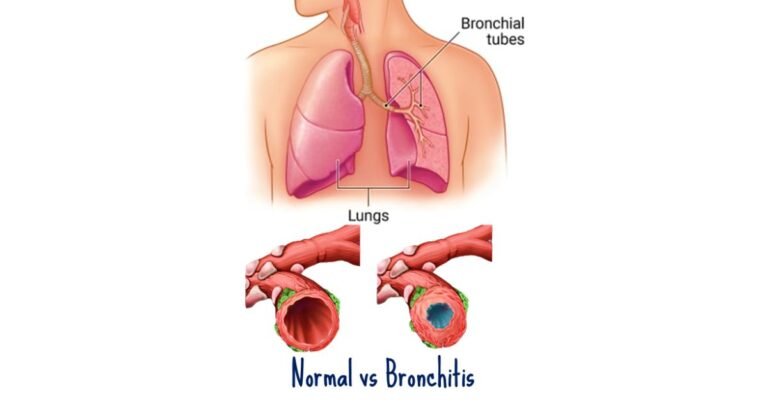
- Interstitial lung disease: Rheumatoid arthritis can lead to inflammation and scarring (fibrosis) of the lungs, known as interstitial lung disease (ILD). ILD can cause symptoms such as shortness of breath, cough, and decreased exercise tolerance. Early detection and management of ILD are essential to prevent progression and optimize outcomes.
- Eye complications: Rheumatoid arthritis can affect the eyes, leading to conditions such as dry eye syndrome, scleritis (inflammation of the sclera), uveitis (inflammation of the uvea), and episcleritis (inflammation of the episclera). These eye complications can cause eye pain, redness, blurred vision, and sensitivity to light if left untreated.
- Increased infection risk: Individuals with RA are at an increased risk of infections due to immune system dysfunction, disease-modifying medications, and comorbidities such as lung disease and diabetes. Infections may include respiratory infections, skin infections, and opportunistic infections in immunocompromised individuals.
- Increased cancer risk: Some studies have suggested that individuals with rheumatoid arthritis may have a slightly increased risk of certain cancers, including lymphoma and lung cancer. Chronic inflammation and immunosuppressive medications used to manage RA may contribute to this elevated cancer risk.
- Psychosocial impact: Living with a chronic disease like rheumatoid arthritis can take a toll on mental health and well-being. Depression, anxiety, stress, and decreased quality of life are common among individuals with RA, particularly those experiencing severe pain, disability, or social isolation.
How is rheumatoid arthritis prevented?
Preventing rheumatoid arthritis (RA) entirely is challenging because the exact cause of the disease is not fully understood, and it involves a complex interplay of genetic, environmental, and hormonal factors. However, there are steps individuals can take to reduce their risk of developing RA or to delay its onset.
- Maintain a healthy lifestyle:
- Regular exercise: Engage in regular physical activity, including aerobic exercise, strength training, and flexibility exercises. Regular exercise helps maintain joint function, flexibility, and overall health.
- Healthy diet: Follow a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and omega-3 fatty acids. Some studies suggest that diets high in antioxidants and anti-inflammatory foods may help reduce the risk of inflammatory diseases like RA.
- Maintain a healthy weight: Obesity is associated with an increased risk of developing rheumatoid arthritis and may worsen symptoms in individuals who already have the disease. Maintain a healthy weight through a combination of diet and exercise to reduce strain on the joints and lower the risk of RA.
- Avoid smoking: Smoking is a well-established risk factor for rheumatoid arthritis and can increase the severity of symptoms in individuals who already have the disease. Quitting smoking or avoiding tobacco use altogether can help reduce the risk of developing RA and improve overall health.
- Manage stress: Chronic stress has been linked to immune system dysfunction and inflammation, which may contribute to the development or exacerbation of rheumatoid arthritis. Practice stress management techniques such as relaxation exercises, meditation, yoga, and deep breathing to help reduce stress levels and promote overall well-being.
- Protect against infections: Some infections have been implicated as potential triggers for rheumatoid arthritis, although the exact role of infections in RA development is not fully understood. Practice good hygiene, avoid close contact with individuals who are sick, and stay up-to-date on vaccinations to help reduce the risk of infections.
- Regular health screenings: Regular health check-ups and screenings can help detect and manage conditions that may increase the risk of rheumatoid arthritis or exacerbate symptoms. For example, individuals with periodontal (gum) disease may be at higher risk of developing RA, so maintaining good oral hygiene and seeking dental care as needed is important.
- Genetic counseling: While genetics play a role in the development of rheumatoid arthritis, having a family history of RA does not necessarily mean that an individual will develop the disease. However, individuals with a family history of RA may benefit from genetic counseling to understand their risk factors and make informed decisions about their health.
- Early diagnosis and treatment: While not a preventive measure per se, early diagnosis and aggressive treatment of rheumatoid arthritis can help minimize joint damage, reduce symptoms, and improve long-term outcomes. If you experience joint pain, stiffness, or swelling, seek prompt medical attention for evaluation and appropriate management.
It’s important to note that while these strategies may help reduce the risk of developing rheumatoid arthritis or delay its onset, they cannot guarantee prevention.
Takeaway
Rheumatoid arthritis is a chronic autoimmune disorder characterized by inflammation of the joints, which leads to pain, swelling, stiffness, and eventually joint damage and deformity. Rheumatoid arthritis is a complex and multifactorial disease, and individual risk factors may vary. Early diagnosis and treatment are crucial for managing symptoms and preventing complications. It’s essential to focus on maintaining overall health, minimizing risk factors, and seeking regular medical care to optimize health and well-being.
Frequently Asked Questions
Q: What are the early signs of rheumatoid arthritis?
A: The early signs of rheumatoid arthritis often include joint pain, stiffness, swelling, and fatigue. These symptoms may start gradually and typically affect small joints like those in the hands and feet.
Q: Is rheumatoid arthritis more common in women than men?
A: Yes, rheumatoid arthritis is indeed more prevalent in women than in men. Women are generally two to three times more likely to develop this condition, though the precise reasons for this disparity are not entirely clear.
Q: Can rheumatoid arthritis go into remission?
A: Yes, rheumatoid arthritis can enter remission, during which symptoms improve or even disappear for a period. Achieving remission often involves suitable treatment, although the disease may flare up again later.
Q: What are biologic drugs, and how are they used to treat rheumatoid arthritis?
A: Biologic drugs are medications derived from living organisms. They target specific components of the immune system involved in rheumatoid arthritis. Typically, they are prescribed when other treatments have failed to control the disease effectively.
Q: Are there any natural remedies or dietary changes that can help manage rheumatoid arthritis symptoms?
A: While scientific evidence supporting the effectiveness of natural remedies for rheumatoid arthritis is limited, some individuals find relief from symptoms through dietary changes. These changes may involve adopting an anti-inflammatory diet rich in fruits, vegetables, and omega-3 fatty acids.
Q: Can rheumatoid arthritis affect children?
A: Yes, rheumatoid arthritis can affect children, although it is less common than in adults. Juvenile idiopathic arthritis (JIA) encompasses the most common form of arthritis in children, including subtypes similar to adult rheumatoid arthritis.
Q: What role does exercise play in managing rheumatoid arthritis?
A: Exercise plays a crucial role in managing rheumatoid arthritis by enhancing joint function, reducing pain and stiffness, maintaining muscle strength, and promoting overall physical and mental well-being. It’s essential to consult with a healthcare professional to develop a safe and effective exercise plan.
Q: Is there a link between rheumatoid arthritis and other health conditions?
A: Yes, rheumatoid arthritis is associated with an increased risk of developing other health conditions such as cardiovascular disease, osteoporosis, and certain infections. Effective management of rheumatoid arthritis may help mitigate the risk of these complications.
Q: Can stress worsen rheumatoid arthritis symptoms?
A: While stress doesn’t directly cause rheumatoid arthritis, it can exacerbate symptoms and contribute to flare-ups. Learning stress management techniques such as relaxation exercises and mindfulness can improve overall well-being and reduce the impact of stress on symptoms.
Q: Is it safe to become pregnant if you have rheumatoid arthritis?
A: Many women with rheumatoid arthritis can have successful pregnancies, but it’s important to consult with a healthcare provider beforehand. This allows discussing potential risks and developing a management plan that ensures the best possible outcome for both mother and baby.