Causes | Symptoms | Diagnosis | Treatment | Complications | Prevention | Takeaway | FAQs
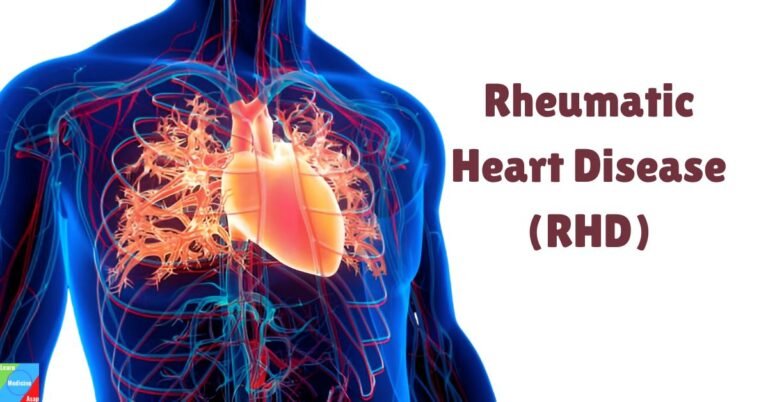
Rheumatic heart disease (RHD) is a chronic heart condition caused by rheumatic fever, which in turn is a complication of untreated or poorly treated streptococcal throat infections. RHD can result in permanent damage to the heart valves, leading to heart failure and other serious health issues.
What is rheumatic heart disease?
Rheumatic heart disease is a long-term consequence of rheumatic fever, which is an inflammatory disease that affects the connective tissues of the body, especially the heart, joints, brain, and skin. The heart valve damage caused by RHD can lead to severe health problems, including heart failure and increased risk of stroke.
What causes rheumatic heart disease?
Rheumatic fever itself is a complication of an infection caused by the bacteria Streptococcus pyogenes, also known as Group A Streptococcus, which primarily causes strep throat and, less commonly, scarlet fever. Understanding the cause of RHD involves exploring the initial infection, the immune response, and the progression to heart damage.
Pathogenesis of rheumatic heart disease
Initial Infection with Group A Streptococcus
The initial step in the development of RHD is an infection with Group A Streptococcus. This bacterium is highly contagious and spreads through respiratory droplets from coughing or sneezing, as well as through contact with infected surfaces. In some cases, the infection causes a sore throat or scarlet fever, which may seem mild but can lead to more severe complications if not treated promptly and adequately with antibiotics.
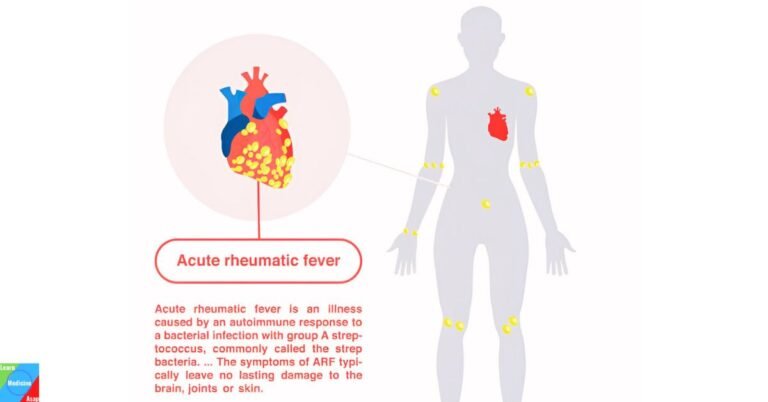
Immune Response and Rheumatic Fever
When a person contracts strep throat or scarlet fever, their immune system responds to the infection by producing antibodies to fight the bacteria. In some individuals, these antibodies can mistakenly target the body’s own tissues, particularly the heart, joints, skin, and brain. This autoimmune reaction leads to rheumatic fever, which typically develops 1-5 weeks after the initial streptococcal infection.
Valve Damage and Chronic RHD
The heart valves, especially the mitral and aortic valves, are most commonly affected by the inflammation caused by rheumatic fever. The repeated inflammation and subsequent healing can lead to scarring and deformities in the valves, resulting in stenosis (narrowing of the valve) or regurgitation (leakage of the valve). Over time, this damage can impair the heart’s ability to function properly, leading to chronic RHD.
Recurrent Infections and Progressive Damage
One of the critical factors in the progression to RHD is the recurrence of streptococcal infections. Each episode of rheumatic fever can cause additional damage to the heart valves, worsening the condition. Therefore, individuals with a history of rheumatic fever are at a higher risk of developing chronic heart disease if they experience recurrent infections.
Risk Factors for rheumatic heart disease?
Several risk factors can increase the likelihood of developing rheumatic fever and subsequent RHD, including:
- Age: Most commonly affects children between 5 and 15 years old.
- Geographic location: Higher incidence in developing countries with limited access to healthcare.
- Socioeconomic status: Overcrowded living conditions and poor access to medical care increase the risk of infection.
What are the symptoms of rheumatic heart disease?
The symptoms of RHD can vary widely depending on the severity of the valve damage and which valves are affected. Some individuals may experience mild symptoms, while others may develop severe complications. The symptoms can be categorized into those occurring during the acute phase of rheumatic fever and those manifesting as chronic heart disease.
Acute Phase Symptoms
During the acute phase of rheumatic fever, which typically develops 1-5 weeks after a Group A Streptococcus infection (like strep throat), the symptoms can include:
Fever: Elevated body temperature is common.
Polyarthritis: Painful and swollen joints, often affecting the knees, ankles, elbows, and wrists.
Carditis: Inflammation of the heart, which can affect the heart’s outer lining (pericardium), heart muscle (myocardium), and inner lining (endocardium). This may present as:
- Chest pain or discomfort
- Heart murmurs: Abnormal heart sounds heard through a stethoscope
- Pericardial rub: A grating sound heard with a stethoscope due to inflammation of the pericardium
Sydenham’s chorea: Involuntary, jerky movements, usually affecting the hands, feet, and face.
Erythema marginatum: A distinctive, non-itchy rash with a ring-like appearance, primarily on the trunk and limbs.
Subcutaneous nodules: Small, painless lumps under the skin, often found near the joints.
Chronic Phase Symptoms
The chronic phase of RHD, which can develop years after the initial rheumatic fever episode, primarily involves the heart valves. The symptoms are related to the type and severity of valve dysfunction, whether stenosis (narrowing) or regurgitation (leakage). Common symptoms of chronic RHD include:
- Shortness of Breath: Difficulty breathing, especially during physical activity or when lying down. This occurs due to the heart’s reduced ability to pump blood efficiently.
- Fatigue: Persistent tiredness and weakness, even with minimal exertion.
- Palpitations: An irregular or rapid heartbeat, which can be uncomfortable and alarming.
- Chest Pain: Discomfort or pain in the chest, which may be more noticeable during physical activity.
- Swelling: Edema, particularly in the legs, ankles, and feet, due to fluid retention.
- Syncope: Fainting or dizziness, which can result from reduced blood flow to the brain.
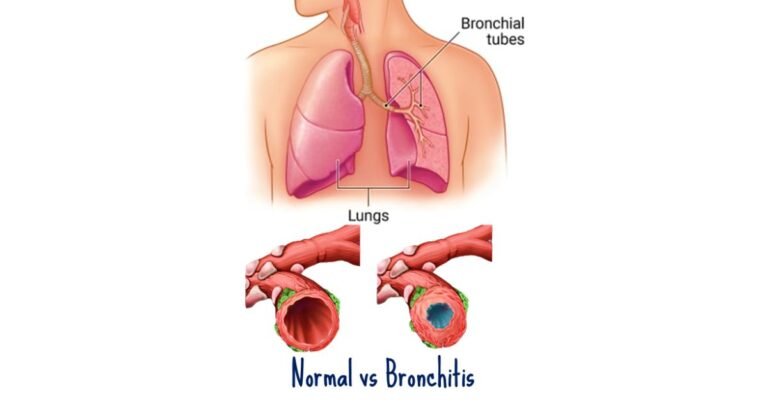
- Persistent Cough: Often a dry cough, which can be caused by congestion in the lungs.
- Hemoptysis: Coughing up blood, which may occur due to increased pressure in the lungs.
- Ascites: Accumulation of fluid in the abdomen, which can cause bloating and discomfort.
How is rheumatic heart disease diagnosed?
Diagnosing RHD involves a comprehensive evaluation that includes a patient’s medical history, physical examination, and various diagnostic tests. Early and accurate diagnosis is crucial to manage the disease and prevent complications. Here is a detailed overview of the diagnostic process for RHD:
Medical History and Symptom Assessment
The first step in diagnosing RHD is obtaining a thorough medical history and assessing symptoms. The doctor will inquire about:
- Past episodes of rheumatic fever: A history of rheumatic fever or untreated strep throat is a significant indicator.
- Symptoms: Detailed questioning about symptoms such as shortness of breath, chest pain, palpitations, fatigue, and swelling in the legs or abdomen.
- Family history: A family history of rheumatic fever or heart disease can also be relevant.
Physical Examination
During the physical examination, the doctor will look for signs of heart valve damage and other indications of RHD, including:
- Heart murmurs: Using a stethoscope, the doctor listens for abnormal heart sounds indicative of valve issues.
- Signs of heart failure: Swelling in the legs, ankles, and feet, along with fluid accumulation in the lungs.
- Skin changes: Observing for signs like erythema marginatum or subcutaneous nodules that are associated with rheumatic fever.
Diagnostic Tests
To confirm the diagnosis of RHD and assess the extent of heart damage, several diagnostic tests may be performed:
a. Echocardiography
Echocardiography, or an echo, is the most important test for diagnosing RHD. It uses ultrasound waves to create images of the heart, allowing doctors to:
- Visualize valve structure and function: Detecting any abnormalities such as thickening, calcification, stenosis, or regurgitation.
- Assess heart chamber size and function: Identifying any enlargement of heart chambers or reduced pumping ability.
- Detect vegetations or clots: Particularly useful in diagnosing complications like infective endocarditis.
b. Electrocardiogram (ECG)
An ECG records the electrical activity of the heart and can help identify:
- Arrhythmias: Irregular heartbeats that are common in patients with valve damage.
- Signs of heart strain: Indicative of chronic heart disease and its effects on heart function.
c. Chest X-ray
A chest X-ray can provide information about the size and shape of the heart and detect fluid in the lungs, which can be signs of heart failure. It helps in:
- Assessing heart enlargement: Enlargement of the heart chambers due to valve disease.
- Identifying pulmonary congestion: Fluid buildup in the lungs as a result of heart dysfunction.
d. Blood Tests
Blood tests can help diagnose underlying or concurrent conditions, such as:
- Markers of inflammation: Elevated levels of C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) indicating inflammation, which can be a sign of ongoing rheumatic fever.
- Streptococcal antibodies: Tests like the antistreptolysin O (ASO) titer or anti-DNase B titer can confirm a recent streptococcal infection.
e. Cardiac MRI
In certain cases, a cardiac MRI may be used to obtain detailed images of the heart’s structure and function. It provides comprehensive information about:
- Heart muscle and valve anatomy: Detailed assessment of valve and myocardial involvement.
- Quantifying heart function: Precise measurement of heart chamber volumes and function.
Differential Diagnosis
The doctor may also consider other conditions that could mimic the symptoms of RHD, such as:
- Congenital heart defects: Conditions present from birth that can cause similar symptoms.
- Other forms of valve disease: Such as degenerative or infective endocarditis.
- Cardiomyopathy: Diseases of the heart muscle that can cause heart failure symptoms.
How is rheumatic heart disease treated?
Effective treatment of RHD aims to manage symptoms, prevent disease progression, and address complications. Treatment strategies can be broadly categorized into medical management, surgical interventions, and preventive measures. Here is a detailed overview of the various treatment options for RHD:
Medical Management
Medical management of RHD focuses on controlling symptoms, preventing recurrent rheumatic fever, and managing heart failure and other complications.
a. Antibiotic Prophylaxis
To prevent recurrent streptococcal infections and subsequent episodes of rheumatic fever, long-term antibiotic prophylaxis is essential. This typically involves:
- Penicillin: Administered either as a monthly intramuscular injection of benzathine penicillin G or daily oral penicillin.
- Alternatives: For those allergic to penicillin, alternatives like erythromycin or sulfadiazine may be used.
The duration of prophylaxis depends on the severity of the disease and the patient’s age, often continuing into adulthood.
b. Anti-inflammatory Medications
During acute rheumatic fever, anti-inflammatory medications are used to reduce inflammation and alleviate symptoms:
- Aspirin or Nonsteroidal Anti-inflammatory Drugs (NSAIDs): To manage arthritis and mild carditis.
- Corticosteroids: In cases of severe carditis to reduce inflammation more effectively.
c. Heart Failure Management
For patients with significant valve damage leading to heart failure, medications are used to manage symptoms and improve heart function:
- Diuretics: To reduce fluid accumulation and alleviate symptoms of congestive heart failure.
- ACE Inhibitors or ARBs: To lower blood pressure and reduce the strain on the heart.
- Beta-blockers: To control heart rate and improve heart function.
- Digitalis: In certain cases, to improve the strength of the heart’s contractions.
d. Anticoagulation Therapy
Patients with certain types of valve disease, particularly those with atrial fibrillation or prosthetic heart valves, may require anticoagulation therapy to prevent blood clots:
- Warfarin: A commonly used anticoagulant that requires regular monitoring of blood levels.
- Newer anticoagulants: Such as direct oral anticoagulants (DOACs), which may be used in some cases.
Surgical and Interventional Treatments
When medical management is insufficient to control symptoms or prevent complications, surgical or interventional procedures may be necessary to repair or replace damaged heart valves.
a. Valve Repair
Valve repair procedures aim to restore the function of the damaged valve without replacing it. Techniques include:
- Commissurotomy: To separate fused valve leaflets in cases of stenosis.
- Annuloplasty: To tighten or reinforce the valve annulus (the ring-like structure supporting the valve).
- Valvuloplasty: Using a balloon catheter to open a narrowed valve (balloon valvuloplasty).
b. Valve Replacement
When valve repair is not feasible or effective, valve replacement surgery may be necessary. There are two main types of replacement valves:
- Mechanical Valves: Made from durable materials, requiring lifelong anticoagulation therapy to prevent clots.
- Bioprosthetic Valves: Made from animal tissues, which do not usually require long-term anticoagulation but may need replacement after 10-20 years.
c. Minimally Invasive Procedures
In some cases, less invasive procedures can be performed to repair or replace heart valves, reducing recovery time and complications. These include:
- Transcatheter Aortic Valve Replacement (TAVR): A procedure for replacing aortic valves without open-heart surgery.
- MitraClip: A device used to repair the mitral valve in patients who are not candidates for surgery.
What are the complications of rheumatic heart disease?
In advanced stages of RHD, complications can lead to more severe symptoms and life-threatening conditions:
- Heart Failure: Severe valve damage can lead to heart failure, characterized by significant shortness of breath, severe fatigue, and fluid buildup in the body.
- Atrial Fibrillation: An irregular, often rapid heart rate that can lead to stroke or heart failure.
- Endocarditis: Infection of the damaged heart valves, leading to fever, new or changing heart murmurs, and blood vessel embolism.
- Stroke: Blood clots formed due to atrial fibrillation or endocarditis can travel to the brain, causing a stroke.
How is rheumatic heart disease prevented?
Preventing RHD primarily involves preventing the initial and recurrent episodes of rheumatic fever. Here are detailed strategies for preventing rheumatic heart disease:
Primary Prevention
a. Early Diagnosis and Treatment of Streptococcal Infections
- Prompt Medical Attention: Seek medical care for symptoms of sore throat, especially if accompanied by fever. Early treatment of streptococcal throat infections (strep throat) can prevent rheumatic fever.
- Antibiotic Treatment: Administer a full course of appropriate antibiotics, typically penicillin, to eradicate the streptococcal bacteria. Alternatives like amoxicillin or azithromycin can be used for those allergic to penicillin.
b. Public Health Measures
- Health Education: Raise awareness about the importance of treating sore throats and completing prescribed antibiotics.
- Improving Access to Healthcare: Ensure access to healthcare services, particularly in low-resource settings where rheumatic fever and RHD are more common.
Secondary Prevention
a. Long-term Antibiotic Prophylaxis
- Benzathine Penicillin G: Monthly intramuscular injections of benzathine penicillin G are the standard for preventing recurrent rheumatic fever.
- Oral Antibiotics: Daily oral penicillin or other antibiotics for those who cannot receive injections. Alternatives include sulfadiazine or erythromycin for penicillin-allergic individuals.
b. Duration of Prophylaxis
- Risk-Based Duration: The duration of antibiotic prophylaxis depends on the severity of heart involvement and the risk of recurrence. Typically, it continues for at least 10 years or until the patient is 21 years old, whichever is longer. For those with severe valve disease, lifelong prophylaxis may be recommended.
Tertiary Prevention
a. Regular Medical Follow-up
- Cardiac Monitoring: Regular echocardiograms and medical check-ups to monitor heart valve function and detect any progression of the disease.
- Management of Complications: Early detection and treatment of complications like heart failure, arrhythmias, and infective endocarditis.
b. Lifestyle Modifications
- Healthy Diet and Exercise: Adopting a heart-healthy diet and engaging in regular physical activity to maintain overall cardiovascular health.
- Avoiding Tobacco and Alcohol: Avoid smoking and excessive alcohol consumption, which can exacerbate heart conditions.
Community and Global Efforts
a. Improving Living Conditions
- Addressing Social Determinants: Reducing overcrowding, improving sanitation, and ensuring access to clean water can help reduce the transmission of streptococcal infections.
b. School and Community Health Programs
- Screening and Treatment Programs: Implementing school-based health programs to identify and treat streptococcal infections early.
Vaccination Research: Supporting research for a streptococcal vaccine, which could significantly reduce the incidence of rheumatic fever and RHD.
Takeaway
Rheumatic heart disease is a serious condition resulting from untreated streptococcal infections. Early diagnosis and appropriate treatment of strep throat are crucial in preventing rheumatic fever and subsequent heart damage. Ongoing medical care and lifestyle management are essential for those diagnosed with RHD to maintain heart health and prevent complications.
FAQs
Q1: What is rheumatic heart disease?
A1: Rheumatic heart disease (RHD) is a chronic condition resulting from damage to the heart valves caused by rheumatic fever. Rheumatic fever is an inflammatory disease that can develop after a streptococcal throat infection (strep throat) and primarily affects children and adolescents.
Q2: How does rheumatic fever lead to rheumatic heart disease?
A2: Rheumatic fever causes inflammation in various parts of the body, including the heart. This inflammation can lead to scarring and damage to the heart valves, impairing their ability to function properly. Repeated episodes of rheumatic fever can cause cumulative damage, leading to chronic rheumatic heart disease.
Q3: What are the common symptoms of rheumatic heart disease?
A3: Symptoms of rheumatic heart disease vary depending on the severity of valve damage but can include shortness of breath, fatigue, irregular heartbeats, chest pain, and swelling in the legs and feet. In severe cases, heart failure may develop.
Q4: How is rheumatic heart disease diagnosed?
A4: Diagnosis typically involves a combination of medical history, physical examination, and diagnostic tests. These tests may include echocardiography (ultrasound of the heart), electrocardiogram (ECG), chest X-ray, and blood tests to detect signs of previous streptococcal infection and inflammation.
Q5: Who is at risk for developing rheumatic heart disease?
A5: Individuals who have had rheumatic fever are at risk of developing RHD, particularly if they have repeated episodes. Children and adolescents in low-resource settings with limited access to medical care and high rates of untreated strep throat are at a higher risk.
Q6: Can rheumatic heart disease be prevented?
A6: Yes, RHD can be prevented primarily by preventing rheumatic fever. This involves early diagnosis and treatment of strep throat with antibiotics, as well as long-term antibiotic prophylaxis to prevent recurrent rheumatic fever in individuals who have already had an episode.
Q7: What treatments are available for rheumatic heart disease?
A7: Treatment options for RHD include medical management, such as long-term antibiotics to prevent recurrent infections, anti-inflammatory medications, and drugs to manage heart failure and other complications. In severe cases, surgical interventions like valve repair or replacement may be necessary.
Q8: What are the potential complications of rheumatic heart disease?
A8: Complications of RHD include chronic heart valve damage (leading to stenosis or regurgitation), heart failure, atrial fibrillation (irregular heart rhythm), infective endocarditis (infection of the heart valves), pulmonary hypertension, thromboembolism (blood clots), and reduced quality of life.
Q9: How long do individuals with rheumatic heart disease need to take antibiotics?
A9: The duration of antibiotic prophylaxis depends on the severity of heart valve involvement and the individual’s risk of recurrent rheumatic fever. It generally continues for at least 10 years or until the patient is 21 years old, whichever is longer. For those with severe valve disease, lifelong prophylaxis may be recommended.
Q10: Is rheumatic heart disease curable?
A10: While the valve damage caused by rheumatic heart disease is often permanent, the condition can be managed effectively with appropriate medical treatment and preventive measures. Early diagnosis and intervention can significantly improve outcomes and quality of life for individuals with RHD.
Q11: Can lifestyle changes help manage rheumatic heart disease?
A11: Yes, lifestyle changes can support the management of RHD. Maintaining a heart-healthy diet, engaging in regular physical activity, avoiding smoking and excessive alcohol consumption, and adhering to prescribed medical treatments can help manage symptoms and prevent complications.
Q12: Are there any global efforts to combat rheumatic heart disease?
A12: Yes, there are global initiatives aimed at reducing the incidence of RHD, especially in low-resource settings. These efforts include improving access to healthcare, enhancing public health education, implementing school-based screening programs, and supporting research for a streptococcal vaccine.
References
- World Health Organization (WHO). (2023). Rheumatic heart disease. Retrieved from https://www.who.int/news-room/fact-sheets/detail/rheumatic-heart-disease
- Mayo Clinic. (2023). Rheumatic fever. Retrieved from https://www.mayoclinic.org/diseases-conditions/rheumatic-fever/symptoms-causes/syc-20354588
- Carapetis, J. R., Beaton, A., Cunningham, M. W., et al. (2016). Acute rheumatic fever and rheumatic heart disease. Nature Reviews Disease Primers, 2, 15084. doi:10.1038/nrdp.2015.84
- Steer, A. C., & Carapetis, J. R. (2009). Prevention and treatment of rheumatic heart disease in the developing world. Nature Reviews Cardiology, 6(11), 689-698. doi:10.1038/nrcardio.2009.162
- Gewitz, M. H., Baltimore, R. S., Tani, L. Y., et al. (2015). Revision of the Jones criteria for the diagnosis of acute rheumatic fever in the era of Doppler echocardiography: A scientific statement from the American Heart Association. Circulation, 131(20), 1806-1818. doi:10.1161/CIR.0000000000000205