Types | Causes | Symptoms | Diagnosis | Treatment | Complications | Prevention | Takeaway | FAQs
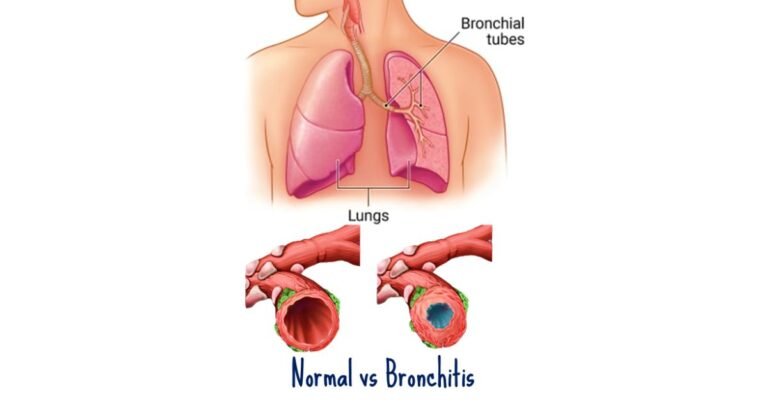
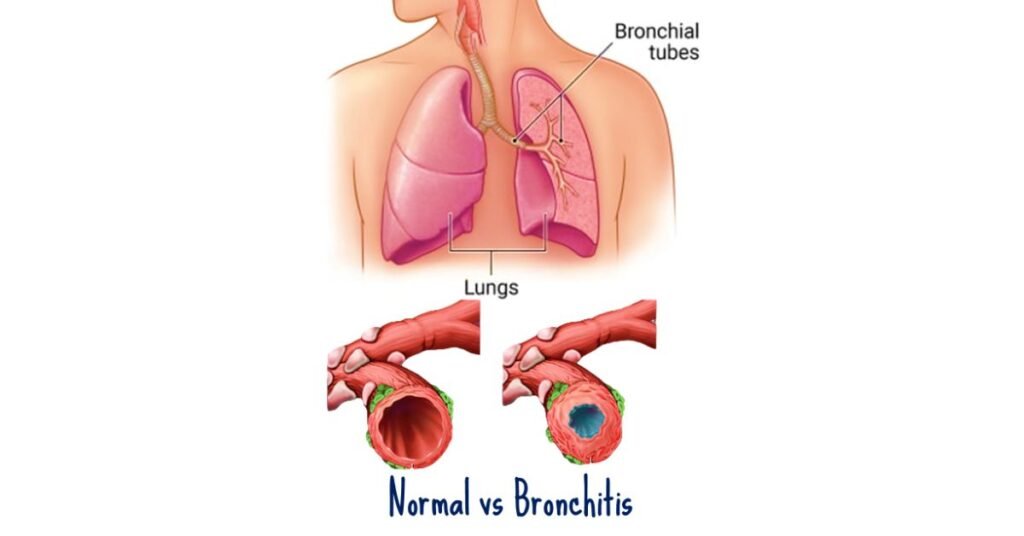
Bronchitis is a respiratory condition characterized by inflammation of the bronchial tubes, which are the air passages that carry air to the lungs. This inflammation often leads to coughing, chest discomfort, and difficulty breathing. It can be acute or chronic, with different causes, symptoms, and treatments.
What is bronchitis?
Bronchitis is a respiratory condition marked by inflammation of the bronchial tubes, which are the air passages connecting the windpipe (trachea) to the lungs. This inflammation can result in excessive mucus production, leading to coughing and difficulty breathing.
What are the types of bronchitis?
There are primarily two types of bronchitis: acute bronchitis and chronic bronchitis.
- Acute Bronchitis:
- Acute bronchitis is usually caused by viral infections, such as the common cold or flu viruses. Occasionally, it can also be caused by bacterial infections or irritants like smoke or pollutants.
- Symptoms of acute bronchitis typically include coughing, often with thickened mucus, chest discomfort or tightness, fatigue, slight fever, and sometimes wheezing.
- While acute bronchitis can be quite uncomfortable, it usually resolves on its own within a few weeks with rest, hydration, and over-the-counter medications to relieve symptoms.
- Chronic Bronchitis:
- Chronic bronchitis is a more serious condition characterized by persistent inflammation of the bronchial tubes. It is often associated with long-term exposure to irritants such as cigarette smoke, air pollution, or industrial fumes.
- Symptoms of chronic bronchitis are similar to those of acute bronchitis but are typically more severe and persistent. Chronic cough with production of large amounts of mucus, shortness of breath, wheezing, and frequent respiratory infections are common.
- Chronic bronchitis is a type of chronic obstructive pulmonary disease (COPD), which is a progressive condition that can lead to permanent damage to the lungs if not properly managed.
- Treatment for chronic bronchitis focuses on relieving symptoms and preventing complications. This may include quitting smoking, avoiding respiratory irritants, using bronchodilators or corticosteroids to improve airflow, and pulmonary rehabilitation programs.
What causes bronchitis?
Bronchitis, whether acute or chronic, can be caused by a variety of factors.
Viral Infections:
- Acute Bronchitis: The most common cause of acute bronchitis is viral infections, often triggered by viruses such as rhinovirus (which also causes the common cold), influenza viruses, adenovirus, respiratory syncytial virus (RSV), and others. These viruses can infect the bronchial tubes, leading to inflammation and irritation.
- Chronic Bronchitis: While viral infections can also contribute to chronic bronchitis, they are less frequent causes compared to acute bronchitis.
Bacterial Infections:
- While less common than viral infections, acute bronchitis can also be caused by bacterial infections, such as Mycoplasma pneumoniae or Bordetella pertussis (which causes whooping cough). Bacterial bronchitis may result in more severe symptoms and may require antibiotic treatment.
Environmental Irritants:
- Acute Bronchitis: Exposure to irritants such as cigarette smoke, air pollution, dust, chemical fumes, or strong odors can irritate the bronchial tubes, leading to acute bronchitis. This type of bronchitis is often referred to as “irritant bronchitis.”
- Chronic Bronchitis: Long-term exposure to environmental irritants, particularly cigarette smoke, is the primary cause of chronic bronchitis. Other occupational exposures, such as working in environments with high levels of dust, fumes, or pollutants, can also contribute to the development of chronic bronchitis.
Allergies:
- Allergic reactions to environmental triggers, such as pollen, mold, pet dander, or certain foods, can lead to inflammation of the airways, exacerbating symptoms of bronchitis, particularly in individuals with allergic predispositions.
Gastroesophageal Reflux Disease (GERD):
- Chronic acid reflux, where stomach acid flows back into the esophagus, can also irritate the airways and contribute to the development of bronchitis, especially in cases where the reflux reaches the lungs.
Immunodeficiency:
- Individuals with weakened immune systems, either due to underlying health conditions (such as HIV/AIDS) or medications that suppress the immune response (such as corticosteroids or chemotherapy), may be more susceptible to respiratory infections, including bronchitis.
Inhalation of Foreign Objects:
- In rare cases, bronchitis can be caused by inhaling foreign objects, such as food particles or small toys, into the airways, leading to irritation and inflammation.
What are the symptoms of bronchitis?
Bronchitis can manifest with a range of symptoms that vary in severity depending on whether it is acute or chronic, as well as individual factors such as age, overall health, and underlying conditions.
- Coughing: Persistent coughing is the most common symptom of bronchitis. The cough may start as dry and irritating but can progress to produce phlegm or mucus, especially in cases of acute bronchitis. The cough may worsen at night or upon waking in the morning.
- Mucus Production: In acute bronchitis, the cough is often accompanied by the production of thickened mucus or phlegm, which may be clear, white, yellowish, or greenish in color. The presence of discolored mucus may indicate a bacterial infection.
- Chest Discomfort or Tightness: Many individuals with bronchitis experience discomfort or tightness in the chest, which can range from mild to severe. This sensation may worsen during coughing spells or with deep breathing.
- Shortness of Breath: Difficulty breathing or shortness of breath is a common symptom, particularly in cases of chronic bronchitis or during periods of exacerbation. This symptom may be more pronounced during physical activity or exertion.
- Wheezing: Wheezing, a high-pitched whistling sound when breathing, may occur due to narrowed airways or inflammation in the bronchial tubes. Wheezing is more commonly associated with asthma but can also be present in bronchitis, especially in individuals with underlying respiratory conditions.
- Fatigue: Bronchitis can cause fatigue or generalized weakness, which may be attributed to the body’s efforts to fight off infection or the increased energy expenditure associated with coughing and breathing difficulties.
- Fever: In some cases of acute bronchitis, individuals may develop a low-grade fever, typically below 100.4°F (38°C). Fever is less common in chronic bronchitis but may occur during exacerbations or if there is an underlying bacterial infection.
- Sore Throat: Sore throat or throat irritation may accompany bronchitis, particularly in cases where the infection extends to the upper respiratory tract. This symptom is more common in acute bronchitis and may precede the onset of coughing.
- Nasal Congestion: Acute bronchitis may be accompanied by nasal congestion or sinus pressure, especially if the underlying cause is a viral infection that affects the upper respiratory tract.
- Chest Pain: Some individuals with bronchitis may experience chest pain or discomfort, particularly when coughing forcefully. This symptom is more common in acute bronchitis and is usually temporary.
How is bronchitis diagnosed?
Diagnosing bronchitis involves a combination of medical history, physical examination, and sometimes additional tests to confirm the diagnosis and determine the underlying cause.
Medical History:
- The healthcare provider will begin by taking a detailed medical history, including asking about symptoms such as coughing, mucus production, chest discomfort, shortness of breath, and any other relevant respiratory symptoms. They will inquire about the duration and severity of symptoms, as well as any factors that may have triggered or worsened the condition, such as exposure to respiratory irritants or recent respiratory infections.
Physical Examination:
- A physical examination is conducted to assess vital signs such as temperature, heart rate, and respiratory rate. The healthcare provider will listen to the lungs with a stethoscope to detect any abnormal breath sounds, such as wheezing or crackles, which may indicate inflammation or obstruction in the airways. They may also examine the throat, nose, and chest for signs of infection or inflammation.
Laboratory Tests:
In most cases of acute bronchitis, laboratory tests are not necessary for diagnosis. However, if the healthcare provider suspects a bacterial infection or wants to rule out other conditions, they may order tests such as:
- Sputum Culture: A sample of mucus coughed up from the lungs may be collected and analyzed to identify the presence of bacteria or other pathogens.
- Complete Blood Count (CBC): A blood test may be performed to assess white blood cell count, which can be elevated in cases of infection.
- Chest X-ray: While not routinely ordered for uncomplicated cases of bronchitis, a chest X-ray may be recommended if the healthcare provider suspects pneumonia or other lung complications.
Pulmonary Function Tests (PFTs):
- For individuals with chronic bronchitis or suspected underlying lung disease, pulmonary function tests may be performed to assess lung function, including measures of airflow, lung volume, and gas exchange. PFTs can help determine the severity of airflow obstruction and may aid in the diagnosis of conditions such as chronic obstructive pulmonary disease (COPD).
Bronchoscopy:
- In rare cases where bronchitis is severe or does not respond to standard treatments, or if there is suspicion of an underlying structural abnormality or lung cancer, a bronchoscopy may be performed. During this procedure, a thin, flexible tube with a camera (bronchoscope) is inserted into the airways to visualize the bronchial tubes and collect samples for biopsy or culture.
How is bronchitis treated?
Treating bronchitis aims to relieve symptoms, manage complications, and address underlying causes such as infections or irritants. The specific treatment approach may vary depending on whether the bronchitis is acute or chronic and the severity of symptoms. Here’s a detailed overview of how bronchitis is treated:
Rest and Hydration:
- Adequate rest and hydration are essential components of bronchitis treatment, especially in cases of acute bronchitis. Resting allows the body to conserve energy and focus on fighting off the infection, while staying hydrated helps to thin mucus and ease coughing.
Medications:
- Bronchodilators: Inhaled bronchodilators, such as albuterol, may be prescribed to help open the airways and improve breathing, particularly in individuals with bronchospasm or wheezing associated with bronchitis.
- Cough Suppressants: Over-the-counter cough suppressants containing dextromethorphan may be used to reduce coughing and ease discomfort, especially if the cough is interfering with sleep or daily activities. However, cough suppressants are not recommended for productive coughs that are helping to clear mucus from the airways.
- Expectorants: Expectorant medications, such as guaifenesin, may be recommended to help thin and loosen mucus, making it easier to cough up and expel from the lungs.
- Antibiotics: Antibiotics are not routinely prescribed for acute bronchitis caused by viral infections, as they are ineffective against viruses. However, if the bronchitis is suspected to be bacterial in origin or if there is a risk of complications, such as pneumonia, antibiotics may be prescribed. Chronic bronchitis may require antibiotic treatment for bacterial exacerbations or secondary infections.
- Anti-inflammatory Drugs: In cases of chronic bronchitis or exacerbations of COPD, corticosteroid medications may be prescribed to reduce inflammation in the airways and improve symptoms.
Nebulizer Treatments:
- In severe cases of bronchitis, particularly in individuals with underlying respiratory conditions such as COPD, nebulizer treatments may be recommended. Nebulizers deliver medication in the form of a fine mist that is inhaled directly into the lungs, providing relief from symptoms and improving airflow.
Humidifiers and Steam Therapy:
- Using a humidifier or steam therapy can help moisten the airways, loosen mucus, and alleviate coughing and congestion. Warm showers or inhaling steam from a bowl of hot water can also provide temporary relief.
Avoiding Irritants:
- Individuals with bronchitis should avoid exposure to respiratory irritants such as cigarette smoke, air pollution, dust, and strong chemicals, as these can exacerbate symptoms and prolong recovery.
Pulmonary Rehabilitation:
- For individuals with chronic bronchitis or COPD, pulmonary rehabilitation programs may be recommended. These programs include education, exercise training, breathing exercises, and nutritional counseling to improve lung function, manage symptoms, and enhance overall quality of life.
Vaccinations:
- Vaccinations against influenza (flu) and pneumonia are recommended for individuals with chronic bronchitis or other underlying respiratory conditions to reduce the risk of respiratory infections and complications.
What are the complications of bronchitis?
Bronchitis, whether acute or chronic, can lead to several complications, especially if left untreated or if underlying conditions are present. While most cases of bronchitis resolve without long-term consequences, complications can occur in certain individuals.
Pneumonia:
- One of the most serious complications of bronchitis is pneumonia, an infection that causes inflammation of the air sacs in one or both lungs. Pneumonia can occur as a complication of acute bronchitis, especially if the bronchial infection spreads to the lungs or if there is an underlying bacterial infection. Symptoms of pneumonia may include high fever, chest pain, productive cough with colored mucus, and difficulty breathing.
Chronic Obstructive Pulmonary Disease (COPD):
- Chronic bronchitis is a common cause of COPD, a progressive lung disease characterized by airflow obstruction and breathing difficulties. Chronic inflammation and mucus production in the bronchial tubes can lead to narrowing of the airways and permanent damage to lung tissue, resulting in symptoms such as chronic cough, shortness of breath, wheezing, and frequent respiratory infections.
Acute Exacerbations:
- Individuals with chronic bronchitis are at risk of experiencing acute exacerbations, sudden worsening of symptoms characterized by increased coughing, mucus production, shortness of breath, and chest discomfort. Acute exacerbations can be triggered by respiratory infections, exposure to irritants, or other factors, and may require prompt medical intervention, including antibiotics or corticosteroids.
Respiratory Failure:
- Severe cases of bronchitis, particularly in individuals with underlying lung disease or compromised respiratory function, may progress to respiratory failure, a condition in which the lungs are unable to provide adequate oxygen to the body or remove carbon dioxide efficiently. Respiratory failure is a life-threatening emergency that requires immediate medical attention and may necessitate mechanical ventilation or other supportive measures.
Cardiovascular Complications:
- Chronic bronchitis and COPD are associated with an increased risk of cardiovascular complications, including heart failure, arrhythmias (irregular heart rhythms), and pulmonary hypertension (high blood pressure in the lungs). Chronic inflammation, hypoxemia (low oxygen levels in the blood), and reduced physical activity levels contribute to cardiovascular strain and may lead to these complications over time.
Decreased Quality of Life:
- Bronchitis, particularly chronic bronchitis, can significantly impair quality of life due to persistent respiratory symptoms, limitations in physical activity, and frequent exacerbations. Breathlessness, fatigue, coughing fits, and recurrent respiratory infections can impact daily functioning, social interactions, and emotional well-being.
Increased Risk of Lung Cancer:
- Although bronchitis itself does not cause lung cancer, chronic inflammation and damage to the airways associated with chronic bronchitis and COPD may increase the risk of developing lung cancer, especially in individuals who smoke or are exposed to other carcinogens such as air pollution or occupational toxins.
Complications in Vulnerable Populations:
- Certain populations, such as infants, older adults, and individuals with weakened immune systems or underlying health conditions, may be at increased risk of complications from bronchitis. Respiratory infections can be more severe in these populations and may require specialized medical care to prevent serious complications.
How is bronchitis prevented?
Preventing bronchitis involves adopting healthy lifestyle habits, minimizing exposure to respiratory irritants and infectious agents, and managing underlying conditions that may increase the risk of respiratory infections.
- Avoid Smoking and Secondhand Smoke: Tobacco smoke is one of the primary risk factors for bronchitis, particularly chronic bronchitis. Quitting smoking and avoiding exposure to secondhand smoke can significantly reduce the risk of developing bronchitis and other respiratory conditions.
- Reduce Exposure to Respiratory Irritants: Minimize exposure to airborne pollutants, such as air pollution, dust, chemical fumes, and industrial smoke, which can irritate the airways and increase susceptibility to bronchitis. Use protective equipment, such as masks or respirators, when working in environments with high levels of respiratory irritants.
- Practice Good Hygiene: Wash hands frequently with soap and water, especially after coughing, sneezing, or touching surfaces in public places. Avoid close contact with individuals who have respiratory infections, and cover the mouth and nose when coughing or sneezing to prevent the spread of germs.
- Stay Up to Date on Vaccinations: Vaccinations can help prevent certain respiratory infections that can lead to bronchitis, including influenza (flu) and pneumococcal pneumonia. Annual flu shots are recommended for everyone aged six months and older, while pneumococcal vaccines are recommended for certain high-risk groups, such as older adults and individuals with chronic medical conditions.
- Maintain Good Indoor Air Quality: Ensure adequate ventilation in indoor spaces to reduce exposure to indoor air pollutants and allergens, such as mold, pet dander, and dust mites. Use air purifiers or filters to remove airborne particles and improve indoor air quality, especially in homes with respiratory allergy or asthma sufferers.
- Stay Physically Active:Regular physical activity can help maintain healthy lung function and strengthen the immune system, reducing the risk of respiratory infections, including bronchitis. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, such as brisk walking, cycling, or swimming.
- Practice Respiratory Health Maintenance: Practice deep breathing exercises, coughing techniques, and airway clearance methods to maintain optimal lung function and prevent respiratory complications. Seek guidance from a healthcare provider or respiratory therapist for personalized recommendations.
- Manage Underlying Health Conditions: Properly manage chronic medical conditions that may increase the risk of respiratory infections or exacerbate bronchitis, such as asthma, allergies, gastroesophageal reflux disease (GERD), and immune system disorders. Follow treatment plans prescribed by healthcare providers and attend regular check-ups.
- Promote Overall Health and Well-Being: Maintain a balanced diet rich in fruits, vegetables, whole grains, and lean proteins to support overall health and immune function. Get adequate sleep, manage stress effectively, and avoid excessive alcohol consumption to promote optimal immune response and reduce the risk of infections.
Takeaway
Bronchitis is a respiratory condition characterized by inflammation of the bronchial tubes, which can cause coughing, chest discomfort, and difficulty breathing. Acute bronchitis is usually caused by viral infections and resolves on its own, while chronic bronchitis is often associated with smoking and can lead to serious respiratory problems over time. Treatment focuses on relieving symptoms and addressing the underlying cause, while prevention involves reducing exposure to respiratory irritants and infections.
Frequently Asked Questions
Q: What causes bronchitis?
A: Bronchitis is commonly caused by viral infections, such as the same viruses responsible for the common cold and influenza. Smoking, exposure to environmental irritants, and weakened immune systems can also contribute to bronchitis.
Q: What are the common symptoms of bronchitis?
A: The typical symptoms of bronchitis include coughing (often with mucus production), shortness of breath, chest discomfort, fatigue, and sometimes fever, especially in cases of acute bronchitis.
Q: How is bronchitis diagnosed?
A: Diagnosis of bronchitis usually involves a combination of medical history, physical examination, and diagnostic tests. Healthcare providers may ask about symptoms, perform a physical exam (including listening to the lungs), and order tests such as chest X-rays or sputum cultures.
Q: What are the treatment options for bronchitis?
A: Treatment for bronchitis focuses on relieving symptoms and addressing the underlying cause. It may include rest, hydration, over-the-counter or prescription medications (such as cough suppressants or antibiotics for bacterial bronchitis), and avoiding respiratory irritants.
Q: What complications can arise from bronchitis?
A: While acute bronchitis typically resolves without complications, chronic bronchitis can lead to serious respiratory problems over time. Complications may include chronic obstructive pulmonary disease (COPD), recurrent respiratory infections, and respiratory failure in severe cases.
Q: How can bronchitis be prevented?
A: Preventing bronchitis involves reducing exposure to respiratory infections and irritants. Strategies include frequent handwashing, avoiding smoking and secondhand smoke, minimizing exposure to air pollution and dust, and getting vaccinated against influenza.
Q: Is bronchitis contagious?
A: Yes, acute bronchitis caused by viral infections can be contagious, particularly during the early stages when symptoms are most severe. It’s important to practice good hygiene, such as covering coughs and washing hands, to prevent the spread of the virus.
Q: What is the difference between acute and chronic bronchitis?
A: Acute bronchitis is a temporary inflammation of the bronchial tubes usually caused by viral infections and typically lasts for a few weeks. Chronic bronchitis, on the other hand, is a long-term condition characterized by persistent inflammation and often associated with smoking or long-term exposure to irritants.
Q: Can bronchitis lead to pneumonia?
A: While bronchitis and pneumonia are two different respiratory conditions, severe cases of bronchitis can sometimes lead to pneumonia, especially if caused by bacterial infections. It’s important to seek medical attention if symptoms worsen or persist.
Q: How long does bronchitis typically last?
A: The duration of bronchitis can vary depending on whether it is acute or chronic. Acute bronchitis typically lasts for a few weeks and resolves on its own, while chronic bronchitis can persist for months or recur over several years, often requiring ongoing management.
Q: Can children get bronchitis?
A: Yes, children can develop bronchitis, especially acute bronchitis, which is often caused by viral infections. Children with underlying health conditions or weakened immune systems may be more susceptible to bronchitis.
Q: When should I see a doctor for bronchitis?
A: It’s advisable to see a doctor if you experience severe or persistent symptoms of bronchitis, such as difficulty breathing, chest pain, high fever, or coughing up blood. Additionally, individuals with chronic bronchitis should seek regular medical care to manage their condition and prevent complications.
References
- “Bronchitis.” American Lung Association. Retrieved from https://www.lung.org/lung-health-diseases/lung-disease-lookup/bronchitis/
- “Bronchitis.” Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/bronchitis/symptoms-causes/syc-20355566
- Simonetti, A. F., Viasus, D., Garcia-Vidal, C., & Carratalà, J. (2011). Management of community-acquired pneumonia in older adults. Therapeutic advances in infectious disease, 3(1), 3-16.
- Patil, M. B., Patil, S. V., Deshmukh, A. D., & Tripathi, S. V. (2016). A review on symptoms, causes, diagnosis, treatment and prevention of bronchitis. Journal of Drug Delivery and Therapeutics, 6(4), 54-59.
- Barnes, P. J. (2010). Chronic obstructive pulmonary disease. New England Journal of Medicine, 363(12), 1128-1138.