Types | Causes | Symptoms | Diagnosis | Treatment | Complications | Prevention | Takeaway | FAQs
Asthma is a chronic inflammatory condition of the airways that leads to breathing difficulties. It involves inflammation, swelling, and constriction of the air passages, making it difficult to breathe.
What is asthma?
Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, resulting in difficulty breathing, wheezing, coughing, and chest tightness. This condition affects people of all ages, from infants to the elderly, and can vary in severity from mild to life-threatening.

What are the types of asthma?
Asthma is a complex respiratory condition that can manifest in various forms, often categorized into different types based on specific characteristics or triggers.
Allergic asthma:
- Allergic asthma, also known as extrinsic asthma, is triggered by exposure to allergens such as pollen, dust mites, mold, pet dander, or certain foods.
- Individuals with allergic asthma typically have a personal or family history of allergies, eczema, or allergic rhinitis (hay fever).
- Symptoms may worsen during specific seasons or upon exposure to allergens, leading to inflammation and constriction of the airways.
Non-allergic asthma:
- Non-allergic asthma, also known as intrinsic asthma, is not triggered by allergens but can be triggered by other factors such as respiratory infections, exercise, cold air, stress, smoke, or strong odors.
- It may develop later in life and is less associated with a family history of allergies or allergic conditions.
- Symptoms may occur more randomly and may not be seasonal or associated with specific triggers.
Exercise-induced bronchoconstriction (EIB):
- Exercise-induced bronchoconstriction, also known as exercise-induced asthma, is characterized by asthma symptoms triggered by physical activity or exercise.
- Symptoms typically occur during or immediately following exercise and may include coughing, wheezing, shortness of breath, and chest tightness.
- EIB can occur in individuals with or without a history of asthma, and it is more common in people who already have asthma.
Occupational asthma:
- Occupational asthma is triggered by exposure to irritants or allergens in the workplace environment.
- Common workplace triggers include chemicals, dust, gases, fumes, or other airborne particles.
- Symptoms may improve when away from work and worsen upon returning to the workplace.
Cough-variant asthma:
- Cough-variant asthma is characterized primarily by a persistent dry cough as the main symptom, without other typical asthma symptoms such as wheezing or shortness of breath.
- Cough-variant asthma can be difficult to diagnose because the cough may be the only symptom, and it may not always respond to standard asthma medications.
Childhood asthma:
- Childhood asthma refers to asthma that develops in childhood, typically before the age of 5.
- Symptoms may include wheezing, coughing, shortness of breath, and chest tightness.
- Childhood asthma can be allergic or non-allergic and often improves or resolves as children grow older.
Adult-onset asthma:
- Adult-onset asthma refers to asthma that develops in adulthood, often after the age of 20.
- It may be triggered by respiratory infections, exposure to allergens or irritants, hormonal changes, or other factors.
- Adult-onset asthma may present differently from childhood asthma and is often associated with more severe symptoms.
Severe asthma:
- Severe asthma, also known as refractory or difficult-to-control asthma, refers to asthma that is not well managed despite high-dose asthma medications.
- It may be characterized by frequent asthma attacks, persistent symptoms, and poor lung function.
- Severe asthma requires specialized management and may involve additional testing and advanced treatment options, such as biologic therapies.
What are the triggers for asthma?
Asthma triggers are substances, conditions, or activities that can exacerbate asthma symptoms or cause an asthma attack by irritating the airways and leading to inflammation and constriction. These triggers can vary from person to person, and understanding and avoiding them are crucial for effectively managing asthma. Here are some common triggers for asthma:
Allergens:
Allergens are substances that can cause allergic reactions in susceptible individuals. Common allergens that trigger asthma include:
- Pollen from trees, grasses, and weeds
- Dust mites found in household dust, bedding, and upholstery
- Mold spores present in damp or humid environments
- Pet dander from cats, dogs, birds, or other animals
- Cockroach droppings and saliva
Respiratory infections:
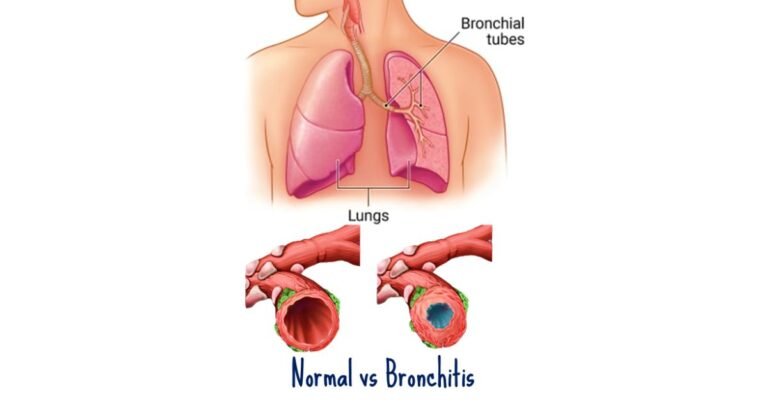
- Respiratory infections, such as colds, flu, sinusitis, and bronchitis, can trigger asthma exacerbations by causing inflammation and irritation of the airways.
- Viral respiratory infections are particularly common triggers for asthma attacks, especially in children.
Irritants in the air:
Irritants in the air can provoke asthma symptoms by irritating the airways. Common airway irritants include:
- Tobacco smoke, including secondhand smoke
- Air pollution from vehicle exhaust, industrial emissions, and smokestacks
- Strong odors from perfumes, cleaning products, paints, and chemicals
- Wood smoke from fireplaces or wood-burning stoves
Exercise:
- Exercise-induced asthma is triggered by physical activity or exercise, especially in cold or dry air.
- Symptoms may occur during or immediately following exercise and can include coughing, wheezing, shortness of breath, and chest tightness.
- Warm-up exercises and using a bronchodilator before exercising can help prevent exercise-induced asthma.
Weather changes:
- Changes in weather, temperature, humidity, or barometric pressure can trigger asthma symptoms in some individuals.
- Cold air can cause airway constriction, while hot, humid air can increase the levels of airborne allergens such as mold and pollen.
Emotional stress:
- Emotional stress or strong emotions such as anxiety, excitement, or anger can trigger asthma symptoms or exacerbate existing symptoms.
- Stress-reduction techniques such as deep breathing exercises, meditation, or yoga may help manage stress-induced asthma.
Occupational exposures:
- Occupational asthma is triggered by exposure to irritants or allergens in the workplace environment.
- Common workplace triggers include chemicals, dust, gases, fumes, or other airborne particles.
- Individuals with occupational asthma may experience improvement in symptoms when away from work and worsening upon returning to the workplace.
Medications:
- Certain medications can trigger asthma symptoms or exacerbate existing asthma, particularly in susceptible individuals.
- Common medications that may trigger asthma include nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin and ibuprofen, beta-blockers, and some pain relievers.
Allergic reactions:
- Allergic reactions to food, insect stings, or latex can trigger asthma symptoms in some individuals, particularly those with allergic asthma.
- Symptoms may include wheezing, coughing, shortness of breath, and chest tightness.
What are the symptoms of asthma?
Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, which can lead to various symptoms ranging from mild to severe. These symptoms can vary from person to person and may also change over time.
Shortness of breath:
- Shortness of breath, also known as dyspnea, is a hallmark symptom of asthma. Individuals with asthma may feel like they can’t catch their breath or are unable to take deep breaths.
- Shortness of breath can occur both during asthma attacks and as a persistent symptom, especially during physical activity or exposure to triggers.
Wheezing:
- Wheezing is a high-pitched whistling sound that occurs when air flows through narrowed airways during breathing. It is a common symptom of asthma and may be audible during exhalation or inhalation.
- Wheezing is caused by the narrowing of the bronchial tubes due to inflammation and constriction of the airways.
Coughing:
- Coughing is another common symptom of asthma, particularly during the night or early morning hours.
- Asthma-related coughing may be dry and persistent, especially in individuals with cough-variant asthma, or may produce mucus (sputum) during asthma attacks.
Chest tightness:
- Chest tightness or discomfort is a sensation of pressure, heaviness, or constriction in the chest.
- Chest tightness may occur along with other asthma symptoms and is often described as feeling like a band tightening around the chest.
- It can be particularly distressing during asthma attacks and may lead to feelings of anxiety or panic.
Difficulty breathing:
- Difficulty breathing is a general feeling of breathlessness or respiratory discomfort that accompanies asthma symptoms.
- Individuals with asthma may experience difficulty breathing due to airway inflammation, bronchoconstriction, or mucus buildup in the airways.
Increased respiratory rate:
- During asthma attacks or exacerbations, individuals may breathe more rapidly in an effort to compensate for decreased airflow through the narrowed airways.
- Increased respiratory rate may be accompanied by shallow breathing or the use of accessory muscles in the neck and chest to aid breathing.
Trouble sleeping:
- Asthma symptoms, particularly coughing and difficulty breathing, can disrupt sleep patterns and lead to insomnia or poor sleep quality.
- Nighttime asthma symptoms may be more common in individuals with poorly controlled asthma or those with nocturnal asthma.
It’s important to note that asthma symptoms can vary in severity and frequency from person to person and may also change over time. Some individuals may experience mild, intermittent symptoms, while others may have more persistent or severe symptoms requiring ongoing management.
How is asthma diagnosed?
Diagnosing asthma involves a combination of medical history, physical examination, lung function tests, and sometimes additional tests to rule out other conditions with similar symptoms. Here is an overview of the diagnostic process for asthma:
Medical history:
- The healthcare provider will begin by taking a detailed medical history, which includes asking about symptoms, their frequency, duration, and triggers.
- They will inquire about any family history of asthma or other respiratory conditions, as well as any personal history of allergies, eczema, or allergic rhinitis.
- Information about previous asthma episodes, exacerbating factors, and response to medications will also be gathered.
Physical examination:
- A physical examination will be performed to assess respiratory symptoms and signs such as wheezing, coughing, shortness of breath, and chest tightness.
- The healthcare provider will listen to the lungs with a stethoscope to detect any abnormal breath sounds such as wheezing or diminished breath sounds.
Lung function tests:
- Lung function tests, also known as pulmonary function tests (PFTs), are crucial for diagnosing asthma and assessing lung function.
- Spirometry is the most common lung function test used to diagnose asthma. During spirometry, the individual breathes into a device called a spirometer, which measures the volume and flow of air during inhalation and exhalation.
- Spirometry measures parameters such as forced expiratory volume in one second (FEV1) and forced vital capacity (FVC). A reduced FEV1 and a decreased FEV1/FVC ratio are indicative of airflow obstruction, consistent with asthma.
Bronchodilator response testing:
- Bronchodilator response testing may be performed as part of lung function testing to assess how the airways respond to bronchodilator medication.
- After baseline spirometry measurements are obtained, a bronchodilator (such as albuterol) is administered, and spirometry is repeated after a short interval (usually 15-30 minutes).
- An improvement in FEV1 of at least 12% and 200 milliliters after bronchodilator administration suggests reversible airflow obstruction, supporting a diagnosis of asthma.
Peak expiratory flow (PEF) monitoring:
- Peak expiratory flow (PEF) monitoring may be recommended for individuals with suspected asthma to assess variability in lung function over time.
- PEF measurements are taken using a handheld device called a peak flow meter, which measures the maximum airflow that can be generated during forced exhalation.
- Regular monitoring of PEF at home can help detect fluctuations in lung function and assess response to treatment.
Additional tests:
- In some cases, additional tests may be ordered to rule out other conditions with similar symptoms or to identify potential triggers for asthma symptoms.
- Allergy testing may be performed to identify specific allergens that could be triggering asthma symptoms.
- Imaging studies such as chest X-rays or CT scans may be ordered to evaluate the lungs and rule out other respiratory conditions.
How is asthma treated?
Treating asthma involves a combination of medications, lifestyle modifications, and education aimed at controlling symptoms, preventing asthma attacks, and improving quality of life. The treatment approach for asthma is typically individualized based on the severity of symptoms, frequency of exacerbations, triggers, and the individual’s response to treatment.
Medications
Bronchodilators:
Bronchodilators are medications that relax the muscles around the airways, helping to widen them and improve airflow. There are two main types of bronchodilators:
- Short-acting bronchodilators (e.g., albuterol) provide quick relief of asthma symptoms during acute exacerbations or before exercise.
- Long-acting bronchodilators (e.g., formoterol, salmeterol) are used as maintenance therapy to prevent symptoms and control asthma on a long-term basis.
Anti-inflammatory drugs:
Anti-inflammatory medications reduce airway inflammation, helping to prevent asthma symptoms and exacerbations. The most commonly used anti-inflammatory drugs for asthma include:
- Inhaled corticosteroids (e.g., fluticasone, budesonide) are the cornerstone of asthma treatment and are used for long-term control of inflammation.
- Oral corticosteroids (e.g., prednisone) may be prescribed for short courses during severe exacerbations to rapidly reduce inflammation.
- Leukotriene modifiers: Leukotriene modifiers (e.g., montelukast) block the action of leukotrienes, chemicals in the body that contribute to inflammation and airway constriction.
- Immunomodulators: Biologic therapies (e.g., omalizumab, mepolizumab) target specific components of the immune system involved in asthma inflammation and may be used for severe, uncontrolled asthma.
Lifestyle modifications:
- Identifying and avoiding triggers: Individuals with asthma should identify and avoid triggers that exacerbate their symptoms, such as allergens, smoke, air pollution, and respiratory infections.
- Maintaining a healthy environment: Creating a clean and allergen-free environment at home, including regular vacuuming, using dust mite-proof covers on bedding, and avoiding exposure to tobacco smoke, can help reduce asthma symptoms.
- Regular exercise: Engaging in regular physical activity can improve lung function and overall health in individuals with asthma. It’s important to choose activities that are well-tolerated and to use a bronchodilator before exercise if needed.
Education and self-management:
- Asthma action plan: Healthcare providers should develop an individualized asthma action plan with their patients, outlining steps to take for daily management and in the event of worsening symptoms or asthma attacks.
- Medication adherence: Ensuring proper adherence to prescribed asthma medications is crucial for achieving optimal asthma control and preventing exacerbations.
- Monitoring symptoms: Regular monitoring of asthma symptoms, peak flow measurements, and lung function tests can help individuals track their asthma control and adjust treatment as needed.
Regular follow-up and monitoring:
- Individuals with asthma should have regular follow-up appointments with their healthcare providers to assess asthma control, adjust treatment as needed, and address any concerns or questions.
- Lung function tests, such as spirometry and peak flow monitoring, may be performed periodically to evaluate lung function and assess response to treatment.
Emergency treatment:
- In the event of a severe asthma exacerbation or asthma attack, emergency treatment may be necessary. This may include the administration of bronchodilators and corticosteroids, supplemental oxygen therapy, and, in rare cases, hospitalization for intensive monitoring and management.
Overall, the treatment of asthma aims to achieve and maintain optimal asthma control, minimize symptoms and exacerbations, and improve quality of life. With proper management, most individuals with asthma can lead active and fulfilling lives.
What are the complications of asthma?
While asthma is a manageable condition for many individuals, it can lead to various complications if not properly controlled or treated. These complications can range from mild to severe and may affect different aspects of a person’s health. Here are some common complications of asthma:
Respiratory infections:
- People with asthma are at an increased risk of developing respiratory infections such as the common cold, flu, sinusitis, and bronchitis.
- Respiratory infections can trigger asthma exacerbations and worsen symptoms, leading to increased inflammation and airway obstruction.
Decreased lung function:
- Chronic inflammation and recurrent asthma exacerbations can lead to a gradual decline in lung function over time.
- Reduced lung function can result in persistent symptoms, decreased exercise tolerance, and an increased risk of respiratory complications.
Severe asthma attacks:
- Severe asthma attacks, also known as asthma exacerbations or asthma flares, can occur suddenly and result in severe respiratory distress.
- Severe asthma attacks may require emergency medical treatment, including administration of bronchodilators, corticosteroids, and supplemental oxygen.
Status asthmaticus:
- Status asthmaticus is a severe and potentially life-threatening asthma exacerbation that does not respond to standard treatments.
- It is characterized by persistent and severe asthma symptoms, including severe shortness of breath, wheezing, and chest tightness, which can lead to respiratory failure if left untreated.
Hospitalization:
- Severe asthma exacerbations may require hospitalization for intensive monitoring and treatment.
- Hospitalization may be necessary to administer intravenous medications, oxygen therapy, and mechanical ventilation in cases of respiratory failure.
Impaired quality of life:
- Uncontrolled asthma can significantly impact a person’s quality of life by limiting physical activity, causing sleep disturbances, and interfering with daily activities.
- Asthma-related symptoms such as coughing, wheezing, and shortness of breath can be distressing and disruptive to daily life.
Psychological impact:
- Living with asthma can be emotionally challenging and may lead to anxiety, depression, or feelings of frustration and helplessness.
- Fear of asthma attacks, concerns about medication side effects, and the impact of asthma on social activities and relationships can contribute to psychological distress.
Medication side effects:
- Some medications used to treat asthma, particularly long-term use of oral corticosteroids, may cause side effects such as weight gain, osteoporosis, cataracts, and increased susceptibility to infections.
- It is important for individuals with asthma to work closely with their healthcare providers to monitor and manage potential medication side effects.
Death:
- While rare, severe asthma exacerbations can be fatal if not promptly treated. Deaths from asthma are often preventable with timely access to medical care and adherence to asthma management strategies.
Overall, the complications of asthma underscore the importance of effective asthma management, including regular monitoring, adherence to prescribed medications, avoidance of triggers, and prompt treatment of exacerbations.
How is asthma prevented?
Preventing asthma involves a combination of strategies aimed at reducing exposure to triggers, minimizing risk factors, and promoting overall respiratory health. While asthma cannot be completely prevented, these measures can help reduce the likelihood of developing asthma symptoms and exacerbations.
Identifying and avoiding triggers:
- Identify and avoid asthma triggers like allergens, smoke, and pollution.
Allergen control:
- Use HEPA filters, wash bedding, and remove carpets to reduce allergen exposure.
Maintaining a healthy environment:
- Keep a clean, well-ventilated home to prevent mold and dust buildup.
Promoting respiratory health:
- Stay active, avoid smoking, eat well, and manage stress for better lung health.
Avoiding respiratory infections:
- Wash hands frequently, avoid sick people, and get vaccinated against flu and pneumonia.
Regular asthma management:
- Follow an asthma action plan, take medications as prescribed, and monitor symptoms closely.
Takeaway
Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, leading to symptoms like wheezing, coughing, chest tightness, and difficulty breathing. It can be managed effectively with medications, lifestyle changes, and avoidance of triggers. Early diagnosis and proper treatment are essential for controlling asthma and improving quality of life.
Frequently Asked Questions
Q: What is asthma?
A: Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, leading to symptoms such as wheezing, shortness of breath, coughing, and chest tightness.
Q: What are the common triggers for asthma?
A: Common triggers for asthma include allergens (such as pollen, dust mites, and pet dander), respiratory infections, exercise, cold air, air pollutants, smoke, and certain medications.
Q: How is asthma diagnosed?
A: Asthma is diagnosed through a combination of medical history, physical examination, lung function tests (such as spirometry), and sometimes additional tests to rule out other conditions.
Q: What are the symptoms of asthma?
A: Symptoms of asthma include wheezing, shortness of breath, coughing, chest tightness, and increased respiratory rate. These symptoms can vary in severity and frequency.
Q: Can asthma be cured?
A: While asthma cannot be cured, it can be effectively managed with proper treatment and lifestyle modifications. Most individuals with asthma can lead active and fulfilling lives with the right management strategies.
Q: What are the treatment options for asthma?
A: Treatment for asthma typically involves a combination of medications (such as bronchodilators and anti-inflammatory drugs), lifestyle modifications, and education about asthma management.
Q: What are the complications of asthma?
A: Complications of asthma can include respiratory infections, decreased lung function, severe asthma attacks, hospitalization, impaired quality of life, psychological impact, medication side effects, and in rare cases, death.
Q: How can asthma be prevented?
A: Asthma prevention involves minimizing exposure to triggers, maintaining a healthy environment, promoting respiratory health, avoiding respiratory infections, and adhering to regular asthma management strategies.
Q: Can asthma attacks be prevented?
A: While asthma attacks cannot always be completely prevented, individuals can reduce their risk by identifying and avoiding triggers, following their asthma action plan, taking prescribed medications, and seeking prompt medical attention for worsening symptoms.
References
- Global Initiative for Asthma. (2021). Global strategy for asthma management and prevention. Retrieved from https://ginasthma.org/gina-reports/
- Mayo Clinic. (2022). Asthma. Retrieved from https://www.mayoclinic.org/diseases-conditions/asthma/symptoms-causes/syc-20369653
- National Heart, Lung, and Blood Institute. (2020). Asthma. Retrieved from https://www.nhlbi.nih.gov/health-topics/asthma
- American Academy of Allergy, Asthma & Immunology. (n.d.). Asthma. Retrieved from https://www.aaaai.org/conditions-and-treatments/asthma
- Asthma UK. (n.d.). Asthma diagnosis. Retrieved from https://www.asthma.org.uk/advice/diagnosis/